Social care technology grew rapidly over the past 5 years. A variety of digital and technical solutions for the range of challenges that care providers face every day. In the rush to provide effective solutions suppliers created a new problem, replacing analogue silos of information with digital ones. The Nourish Partnership Programme addresses this problem by building a comprehensive digital estate of integration partners, that our users can review and apply to their service as required, so they can continue to provide outstanding care for their communities.
‘We need to talk’ – a sentence that sends shivers down spines in bedrooms and boardrooms alike. Feedback acquisition, data gathering, internal research—whatever you name the process, conversation is critical to success. In social care, conversations are a fundamental part of providing quality, person-centred care. Care providers learn the best information about the people who utilise their service by engaging directly with them. Our partners, ImproveWell, build upon this opportunity by offering simple, easy-to-apply engagement tools for your workforce, clients and wider stakeholders.
Knowledge is power and ImproveWell gives you the power to prepare for inspections, increase employee engagement and drive qualified, person-centred improvement across your service.
The Care Quality Commission in England has been rolling out its new inspection process since November 2023. The ‘single assessment framework’ is designed to put people at the heart of the inspection process. While the key categories remain the same; safe, caring, efficient, well-led and responsive, the methods for evidence gathering are updated. There are six categories for evidence that inspectors will now require.
The first three – ‘people’s experience of health and care services’, ‘feedback from staff and leaders’ and ‘feedback from partners’ – are all different forms of conversations. ImproveWell helps your team prepare for these conversations. By making real-time feedback simple and a regular occurrence in your care community by providing a mechanism for feedback anytime, anywhere. You can gain a clearer, and more regular insight into the experiences of your organisation at every level. Without even getting into the results of your engagement activities. Simply introducing the process to your teams and community will make them more familiar and, in doing so, more comfortable with it.
The latter three categories – observation, processes and outcomes – can all be improved through utilising the results of ImproveWell’s functionality. ImproveWell’s solution can be set up in a bespoke way to suit the needs of your team and service. Everyone can suggest ideas for improvement, share how their workday is going, and complete tailored pulse surveys – 24/7. Insights from wider stakeholder groups can be gathered and an AI-powered data dashboard enables group and organisational leads to monitor real-time data, track workforce sentiment, prioritise quality improvement efforts, measure change, and publish reports to complete the feedback loop.
The Maternity Department at Royal Cornwall Hospitals NHS Trust enjoyed notable improvements to their workforce engagement and morale. After the first phase of ImproveWell’s introduction in the Maternity Department. 75% of staff reported feeling able to improve their area of work, compared to the 53% scored by the Trust as a whole. (2018 NHS staff survey) Moreover, over 85% of users of ImproveWell felt it empowered them to implement ideas for change.
This is what makes these tools so relevant to inspections outside of England as well. All inspectors will engage with your staff in one form or another as part of their process. Whether it’s in their ear or over their shoulders. The more familiar the workforce is with being listened to and respected by senior management, the better they can provide and evidence high-quality care.
The Maternity Department at Royal Cornwall Hospitals NHS Trust were able to improve their CQC rating from ‘Inadequate’ in 2017 to ‘Requires Improvement’ in 2018 following their implementation of Improvewell. In November 2019, the Maternity Department won the International Maternity Expo Transformation Innovation Award to recognise achievements made through ImproveWell, and in their most recent inspection in February 2023, they had improved the ratings for ‘Safe’ and ‘Well-Led’ to ‘Good’.
Workforce engagement is crucial in social care. We know that high job vacancies and staff turnover rates are longstanding issues for care providers. One of the surest ways to draw a big audience at any care event is to talk about recruitment and retention. It’s obvious if you have attended any of these talks in the past few years. You will know more and more providers are looking to improve their staff retention rates by increasing their employee engagement.
“We’ve learnt that everyone would like more money but surprisingly it’s not as important as being happy in their work. Support and development of people is held in higher regard.” Residential care provider, Claxton House, Atlanta Healthcare.
The best way to support and develop people is to listen to them. Of course, that’s generally much easier said than done. ImproveWell turns recording, reviewing and actioning ideas from your workforce into a smooth, seamless process. The detail and specificity of ImproveWell’s functionality enables you to ask the right questions. Crucially, the AI-powered data dashboard provides an easy-to-use, insightful overview of the information you have gathered, so you can use frontline feedback for maximum effectiveness. Most care providers conduct internal surveys with their team, with varying results. ImproveWell enables you to take these findings further, and action them to the benefit of your service by empowering your team and wider community to take a more active role in their development, in both a personal and professional capacity.
Health and care providers who use ImproveWell to engage with their community have noticed benefits in four key areas. The first, and most direct benefit, is the increase in staff wellbeing and morale. It is only natural that satisfaction increases and turnover decreases when people feel like they play an active and important role in their workplace.



Users also experience a notable quality improvement, in terms of the care they are able to provide. Primary sources are always the best place to start when looking to improve your processes. It is the people who are directly involved who have the deepest understanding, whether they are providing care, utilising care, or are a member of the community in which you operate. A wealth of insight is unlocked when you empower your community to be actively responsible for their care.
“It’s the quick fixes that make the difference,” Nicole Lee, Chelsea and Westminster Hospital NHS Foundation Trust Burns Service, Burns Matron.
This same logic applies when it comes to your service’s operational and cost efficiency. It is impossible to fully understand something by looking at it from the top down. All leaders know they need multiple perspectives to understand their organisation. Increase your operational and cost efficiency by creating a simple route for innovation. Carers are known for making a little go a long way, harness their ingenuity and experience and the rewards will soon follow.
People are the pulse of our communities. Engage directly with them to best understand the world in which your service exists. The concept behind micro-improvements is rooted in experience and the belief that with the right knowledge, you have the power to change the world. Maybe not the whole thing, but definitely your own. However first, we need to talk.
At Nourish Care we’re committed to continuously improving the accessibility and inclusivity of our technology, working towards our goal of developing a solution which truly works for everyone. We spoke to our Head of Product Design, Kate Horn, to learn more about our approach to embedding accessibility and inclusivity at the heart of our product design process.
“Accessibility and inclusivity have accidentally become a bit buzzwordy in the design world recently,” explains Kate, “and most definitely in health tech design. Why? Finally, we are all talking about ensuring that anyone can access the products we are creating. At Nourish these are not just words, they form the basis of design values that go right to our core, we are person-centred. We believe in a better life for everyone. To achieve this, we need to make sure anyone and everyone can use Nourish.”
“Honestly? They mean quite a lot of different things!
“It is a common misconception that when we talk about accessibility, we are only talking about how we apply colours to designs and how we can make it high contrast. This is a factor, but it barely scratches the surface of the work to be done to make a platform, or an app genuinely accessible to anyone who wishes to use it.
“Hold on a moment though, we are talking here about using something that is in your hand already. We need to take a step back and think about the technology and very basic level of access first and how, as designers, we can get the app into your hand or onto your desktop in the first instance. Given that you are reading this digitally, this is clearly not a problem for you but consider this; in 2022, 13-19 million people in the UK over 16 lived in a state of digital poverty. That means they did not have the tech, skill, or resources to fund internet access on one or more occasions a week.



We cannot just build for the latest and most shiny versions of everything. Accessibility means we need to think about making sure what we create is available to everyone. In a way which does not exclude people, starting at the point of access and empowering them to enjoy the full experience of the platform.
“Inclusive” needs to go even further and it is worthy of a blog post on its own. For now, I want to touch on the importance of ensuring that inclusivity extends to individuals feeling genuinely included, seen and represented within our platforms.
First of all, we aim for the highest possible standard. There is a framework for accessibility in digital design for us to follow called WCAG. Within this there are levels, the highest of which is standard 2.2. This is what we strive to achieve. Standard 2.2 covers everything from the use of text, audio, layout, contrast, colour, platform adaptations, use of imagery, operational considerations, inputs, consistency of design and ensuring the platform is robust. And that’s just to start!
It is a solid start, however, a framework does not go far enough for accessibility and it doesn’t answer the requirement for inclusivity. To achieve this, there are several other elements to consider, starting with words.
Words are a powerful way for us to be both engaging and human, when used correctly. They are also one of the quickest ways for us to disconnect people from Nourish. If we describe areas of the platform or tasks using inhuman or technical language you first have to understand what we really mean and then have to choose if you really want to do it. We’re to make things simpler for you, not more complicated! So, step one for us is to speak in common English and start to create a comfortable experience.



Next on that list is understanding who we are designing for. This requires us to become so embedded in the health and care sector that we are a part of the furniture. Great insight means we understand the everyday challenges the people who are using our platform experience. This ensures we craft experiences for our platforms that work to solve these problems in a way that is comfortable for everyone.
Throughout this blog I have used the words “anyone” and “everyone”. These are crucial terms for defining our approach. Typically, designers aim to design for the bell curve, that is, the biggest group of users.
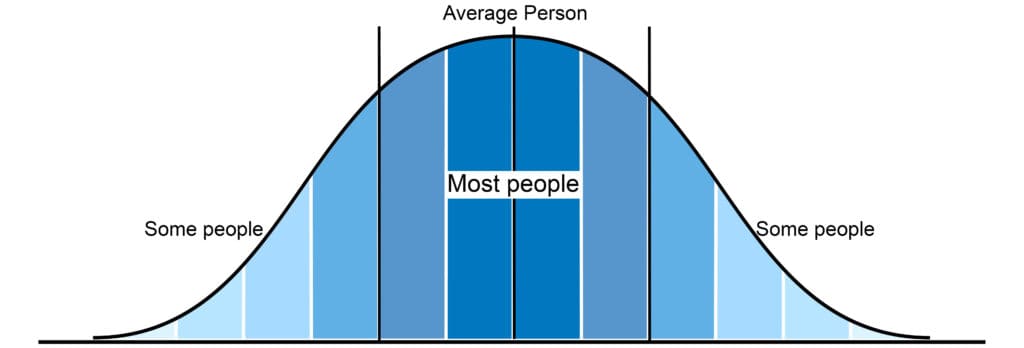
We simply cannot do this in health and social care. We have to step back and design solutions that truly work for anyone. This “flattening” of the curve is really important. It goes to the core of what we work to achieve as a company and the heart of our values as a design team. We want to create technology to truly wrap around the user in a great experience.
As users of Nourish will know, we’re continuously improving the accessibility and inclusivity of the platform, these really aren’t just buzzwords to us. We are working towards our goal of creating a system which can be easily used by anyone. There’s always more that can be done but by keeping these principles and our users at the heart of our design processes we are able to keep our person centred goals firmly in sight.
Book a demo to find out more about Nourish and how we can work with anyone, and everyone in your community.
Social care is in a state of change. Care providers tasked with being the steady hand through this change have consistently risen to the challenge. Despite having little control over the changes as they happen. At Nourish Care we are embracing this change by working with our users to develop a social care future we are all proud of. With increasing standards, new regulations and extended funding availability it is clear now why so many care providers are embracing change themselves and switching to Nourish.
Care providers have a wealth of options when choosing a digital partner. Under the original standards for the NHS Assured Solutions List (ASL) there are 24 Digital Social Care Records (DSCRs) to choose from. That’s without mentioning the systems who don’t reach these standards. The ASL is enjoying notable success so far, as it continues to work towards its target of 80% of care providers on DSCRs. Digitisation is widespread through social care now. To the point that many care providers are shopping around for a better system to match their service.
The ASL was always intended as a starting point for the digitisation of social care. The Department of Health and Social Care has announced the second step of this journey, with the recent release of the 14 new standards for DSCRs on the ASL. We are one of the few providers to have achieved all 14 of these standards. You can read about the specifics of the standards here.
We are the largest software supplier to have achieved the new standards. As well as being one of the first to get listed on the ASL following its initial launch. Our legacy of forward thinking and innovation consistently aligns us with the future direction of the social care sector. We are proud to be working closely with key decision makers in health and social care.
We support care in a huge variety of settings. Including older person’s care, nursing, home care, learning disabilities, dementia, supported living, assisted living, substance abuse, mental health, children and young people and more. Each care setting is unique, and each care setting requires specific understanding to support effectively.
Our experienced and understanding customer success and support teams will work with you to make sure our system fits your service. Whatever your needs are, and whatever they may become in the future.
Once you switch to Nourish, we are with you every step of your journey. Should your journey lead you to new business opportunities we are the best equipped software supplier in social care to support your expansion. Whether you are focussed on a single type of care or support a range of different needs.
You can also scale your functionality as desired, thanks to our comprehensive partnership programme. The programme unites key best-in-class innovators like Camascope for eMAR, Radar for incident management and PainChek for pain management. All while keeping a finger on the pulse for emerging technologies that will substantially impact the social care sector.
Additionally, we offer more in-depth data packages called ‘Insights’ and ‘Analytics’. These features provide a much richer insight into the data gathered across your service. Perfect for larger care providers who collect vast swathes of information every day, but have no clear way to transform this potential into insightful, actionable information.
The Care Quality Commission’s (CQC) rollout of their new Single Assessment Framework (SAF) is enduring some understandable teething challenges. Initialisms aside the ambition of the project remains clear. The regulator wants to streamline processes and better respond to the needs of the people who draw upon care.
We facilitate these new developments as effectively as possible. We work with organisations like the Care Software Providers Association (CASPA) to share our voice and insights on the development of digital social care with key decision makers in local and national government. Our work on alignment with #socialcarefuture helps to guide the future of our system as much as they guide the future of the wider care communities. Socialcarefuture are the co-authors of the ‘I/We Statements’ that define the SAF scoring.
There is always something new to be considered, a fresh function to be explored or a new piece of legislation to be adhered to.
We cannot know the future; all we can do is prepare for it. We have read the tea leaves, built our houses from stone and made hay while the sun shone. All so we can continue to lead the way in digital social care, through innovation, understanding and collaboration.
Social Care is in a state of change, and with that ever-present uncertainty comes a great opportunity. Switch to Nourish today and take control of your change, with your team, your service and your community.
Teamwork makes the dream work, though a good partnership is hard to find. At Nourish Care we are committed to working with our users throughout their digitisation journey. A journey that continues beyond tomorrow’s horizon and into the future of care. The results of our partnerships are present for the over 400,000 people who are cared for with Nourish software solutions. People define partnerships, and by putting partnerships at the centre of our approach we ensure that people are always our focus.
From the moment you first speak to Nourish there will be someone on our side working with you. Every step of your journey. This applies to care providers of all shapes, sizes and disciplines.
Digitisation can take time, whether you are looking to reshape systems or just starting off your journey. We make sure all our users have the right guidance alongside them to make this process as smooth as possible for your team and as specific as necessary for your community.
Project managers are available to help care home groups and large franchises transition to Nourish. They work with your team to ensure an effective digital rollout. We have dedicated customer success managers to work with medium and smaller care providers, as well as being another helping hand for large groups. These managers are adept at supporting the unique needs that emerge when providing care for your community. They know how to guide our users during their set-up process to ensure you receive the maximum benefits from Nourish.
Our partnership doesn’t end at the onboarding. We continually work with our users. Offering you an open line and a dedicated point of contact for your service, so you can continue to grow the way you want to and flourish with Nourish. You can read more about how Nourish has supported the teams and growth of home care providers Nexus Care and Priory Group’s care homes.
Visit our Case Studies page for more examples.
Expertise is essential to success, and our partnerships with services excel at combining our knowledge with yours. We have researched and developed robust libraries alongside care and clinical professionals with a deep understanding of the sector and needs of the population. Each library contains interactions, assessments, care plan templates and more for managing specific pathways, conditions, needs and day-to-day operational requirements.
We combine this wealth of best practise and experience with your understanding of your community’s needs. Nourish boasts a depth of customisability. This promotes the individuality of your service in line with the established requirements of commissioners and regulators. The only assets that are not customisable are locked to ensure compliance with a particular protocol or standard. This empowers your coordinators to wrap your system around your service and provide for the specific needs of your community.
There is a reason we are the largest software supplier for social care in the UK. We do not settle for general. Nourish is filled with functionality that supports the unique requirements of different care types. Including residential, domiciliary, nursing, assisted living, learning disabilities and many more.
Strong rostering is the backbone of efficient home care management. We built our rostering with over a decade of experience working with home care providers. It can be set up on repeating schedules of up to a month. Our drag and drop rostering and customisable carer rating system gives you the tools to quickly adapt to changing circumstances with your workforce and the people they support. Your rostering can then be simply invoiced and time-sheeted with our comprehensive finance functionality. Ensuring you pay everyone the right amount at the right time.
Nourish’s mobile app for home care is another product of our strong partnerships with care services. We work with providers to keep our app up to date and empowering their care teams and communities. Carers know where they’re going and what they’re doing, while keeping you up to date on how it went through their appointment notes and audit tracker. Travel times, upcoming schedule, care types, medications and notes are all designed alongside carers and available offline. So your team have everything they need, anywhere they go.
Nourish is designed by care professionals for busy care environments, combining icons, imagery and text to create a smooth, easy experience. Keeping carers informed is crucial in residential settings as well. The care plan summary on our care home mobile app provides a detailed and concise snapshot on mobile for a particular need to ensure nothing gets missed and you have all the information available. Carers have access to all the information on the mobile app which empowers care teams. They can see the handover, review recent and historic appointment notes. A level of autonomy unrivalled by any other DSCR platform. The app also features ‘back’ and ‘save’ buttons wherever you go so no records can be lost when completing a record/interaction.
Data is a hot topic, but one that has burnt the finger of many a service. With Nourish managing data can become a simple part of your daily process. We provide several prebuilt dashboards within our system to provide data oversight to your team. These dashboards can become a cornerstone or a starting off point for your team’s application of data. We have experienced people on our team to help you get what you need from your data in your reporting. So you can focus on providing, responsive, effective care.
All of our success at Nourish has come through collaboration. Collaboration between our teams, between our integration partners and between our users. We believe the best solutions are produced through teamwork. A process without an end, but an enduring, enjoyable journey. We’re in this for the long haul, with true partnerships, the lasting kind.
New technology in care is revolutionising the way we support people and artificial intelligence is quickly making an impression on the social and health care sectors. From the latest smartwatches recording our morning runs to electronic care planning systems and even robot surgery! New innovative tech systems and devices are collecting data and analysing trends to identify patterns, and cross-referencing patient data in order to gain quick and reliable insight. While some are celebrating AI’s ability to revolutionise the way we care, many still fear this technology and see it as a threat to their personal security, something we have looked at previously ‘Electronic Care Planning: Change Doesn’t Need to Be Feared’
A large part of this fear is down to education, and in order to encourage not just care professionals, but anyone and everyone who interacts with the world of care, to have confidence in these technologies, it’s important to highlight the great benefits that they offer to the lives of those we love and care for.
In this article, we’ll be looking at some of the latest technologies that are enhancing the world of care management through data analysis and the well-being of those in care.
One of the new technologies we are seeing revolutionising the way we care is Virtual Reality (VR) headsets, which could soon become standard in dementia care homes. More than just a form of entertainment, some recent small studies suggest that VR environments could help trigger old memories in seniors, helping to make them feel less alone and confused.
Not only does this have positive effects on those living with dementia, but it improves their relationship with their carers and families too. It can reduce aggressive behaviour in patients and allows carers to gain better insight and understanding of those they’re caring for, thus improving caring interactions.
The FDA has recently approved the first version of a Glucose Monitoring System, which can be implanted just below the skin and has a sensor that can be worn for up to 90 days. These systems continuously monitor sugar levels and send data to a display device, and they also allow you to set up alerts for high, low or significant changes.
This will allow carers to monitor those with chronic diseases like diabetes much more closely, including during the night, and they can track trends in changes to sugar levels. A CGM also reduces the need to do finger prick tests and allows you to administer more accurate doses of insulin. Ultimately this device enables carers to act quicker and care better.
5G is quickly changing the efficiency of social care. With analogue signals soon to be switched off, 5G will allow much faster, safer and more reliable handling of data. 5G offers speeds up to 10 x faster than 4G, and it’s being used in a number of ways to provide support, including remote monitoring.
Remote monitoring can benefit elderly or vulnerable groups who receive care as it can reduce the number of trips they need to take to the hospital. Care professionals can receive and analyse data, as well as share data securely and in real time. Devices powered by 5G could help carers detect problems earlier, and refer and exchange data with other care professionals for more accurate and better quality care.
Smart technology has been on the scene for a little while now, but it remains one of the leading technologies revolutionising the way we care. Homes are kitted out with everything from smartphones to energy meters and assistive technology like Alexa or Google. And this is no different in a care environment. Carers are quickly beginning to adopt a digital way of working, using electronic care planning systems (like Nourish), to enhance the way they care.
Many organisations in the care sector are now seeing the benefits of going paperless. Not only is it more environmentally friendly, but it allows for far more accurate data capturing, recording at the point of care, and most importantly, more person centred care because staff are no longer having to take hours doing admin tasks.
While many of these technologies may still seem like something from the distant future, 2020 is seeing a far more encouraging approach to integrating into the world of digital, with some of these things already being used by social and healthcare professionals.
Technology in Social Care…
Since Kate Terroni became Chief Inspector this Summer, I have been reflecting on how a new person in that post would see their role in promoting innovation in the care sector. It was with childlike excitement that I read Kate’s latest blog post. In this, Kate describes how she has been shadowing some of her inspectors and her findings – and it was fantastic to get her initial thoughts on the use of technology by care teams.
“Speaking with carers I have found that this technology means they can spend more time with the people they support and less time doing paperwork — a welcome benefit of technology.”, Kate Terroni, Oct 2019
And what is the most refreshing is the clarity of thought on the difference between “using technology” and “innovation”, something that resonates immensely with how we see the world at Nourish.
We have long been believers that carefully designed technology, with the right associated services, can enable a whole range of cultural changes. Including how care teams perceive their own ability to drive innovation. It is important that care teams don’t develop a perception that innovation is something you buy. It is not.
Care teams showing CQC what good technology can achieve is a wonderful demonstration that technology makes a difference for them. It hasn’t always been this way.
Going forward it’s important to acknowledge that for a long time, many people misunderstood the potential for technology in Social Care. With a dozen challenges constantly putting pressure on care teams, the prospect of making a big change such as embracing digital tools for managing care has often filled people with dread – which is very understandable. And historically it wasn’t just for fear of change that care teams have put this off.
The maturity of the products available has come a long way in the last 5 years. Prior attempts to adopt technology by care teams invariably resulted in frustration – products that looked amazing in the eyes of a manager or the owner of a care home ended up requiring hours of training for care workers with clunky user experience, poor customer support, resulting in failed uptake, and a background feeling that “technology doesn’t work in social care”. Care workers were never heard in the process of choosing digital tools, and the introduction of technology was often done in the assumption that it would “help the numbers by making carers more efficient” – as if efficiency could be introduced by some sort of industrial process of optimisation. Thankfully, the sector and the technology that supports it have moved on.
Like any context that is as complex and nuanced as social care, the thought of designing technology at arm’s length resulted in oversimplified solutions often shaped within a software team which would then sell it as fast as possible – this was never going to work. So, what is it about social care that is so different from, say, healthcare? Why can’t we just use a personal health record and expand it?
Well, we can’t. We can’t because social care is not just about someone’s condition or frailty. Good social care services support the person as a whole. And people are extremely diverse – society as a whole is learning that there is no such thing as a template for an “older person” – as we have more people living longer our cultural stereotypes of what is an “older person” are crumbling – older people are “people” – we can’t stereotype them. And therefore, there is no universal template for an Older Person’s Care Plan. Good social care for a person living with frailty supports the person in a way that is aware of the whole person – not just of their frailty. And whereas a person has dozens of encounters with healthcare services in a year, the same person may have dozens of encounters with their care team in a single day.

Care Plans are as diverse as the people they are designed to support.
So, having spent 6 years continuously co-designing Nourish with hundreds of care providers, it’s no surprise care teams feel so different about us. We are not a “technology” company. We are a company that uses a software product and services to make care teams feel empowered to improve and innovate in the context of the care they provide. Carers don’t need to sit on training sessions for hours, it’s intuitive technology that allows them to understand the context of a person, know how to support and what’s important for the person, record naturally as part of providing support rather than “doing record keeping at the end of the shift”, and feel empowered. Empowered because they can spend more time with the people they support. And in addition, from knowing their residents better, they can continuously innovate, suggest adjustments to support plans, identify shifts in personal preferences or suggest new activities that are likely to improve the quality of life for each person.
Innovation happens when care providers design new and better ways to discharge people from hospital, or when they find different ways to enable people to go on a holiday, fulfil a last wish, increase their comfort, find or revive a sense of purpose, supporting every person, old and young, to be and feel the best they can feel.
Technology that enables care teams to do this, will be at the heart of all good care teams in the future. And we are delighted to see the Care Quality Commission so clearly sharing our vision on this.
Could technology help your care service?
Find out more about whether using an electronic care planning could help you and those you support here.
Care providers far and wide are already making the transition to digital care management; benefiting from higher quality care plans and notes, compliant and accurate audit trails and a greater degree of control across the management process.
These benefits are being felt at every level, from care managers and carers to the people they care for and their families. Here, we talk to three experienced care providers about the individual impact Nourish Care is having across the entire care service.
For carers, Nourish is empowerment at the point of care. By using well designed and easy to use applications on handheld devices, carers can record notes as they go.
Carers are thereby able to focus a lot more on the person they are working with, and encouraged to record the person-centred care notes that inspectors say distinguishes a care service. Recording notes alongside care also promotes greater clarity, adds useful context and ensures all information is recorded as soon as possible – not forgotten over the course of the day. Recording as they go, carers have the opportunity to really demonstrate the great quality of care they are giving.
Simon Francis, IT Project Manager at Silverline Care, commented: “The main thing for our carers is that the recording of notes is a lot easier. What they were doing beforehand was having to provide care and then try and hold all that information until the end of the shift. Care for residents is now much more to the point and accessible. There is better communication between staff and everyone involved in the client’s care can see what care has already been provided by others. This has made handover a lot easier. It also means input from the carers feeds directly into the care plan, meaning it’s updated within minutes of it taking place. Recording in real time means we don’t lose any important information.”
Paul Dennis-Andrews, Operations Manager at Encompass, has been working with the Nourish Care since spring 2016. He added: “The digital care management system has had a highly positive impact on the overall culture of our service – more than we ever would have thought. Staff who might have had difficulties with the written word are enthused by the ability to speak verbally into the devices to record information. It has been a refreshing and efficient change to a longstanding process of handwritten documentation.
“The large collection of paper files has been replaced with discrete modern handsets and tablets that staff can keep on their person, promoting highly person-centred support exactly how the individual would like to receive it. Documentation is recorded live and visible immediately to anyone with permission, and every aspect of the system is customisable and can be evolved to needs.”
Probably one of the biggest benefits for senior carers and care managers is that all information is in one place and accessible at any time. Care notes and assessments feed directly into the care plans and can be accessed by all who need to see them. This develops a culture of knowledge-sharing and allows for more effective care monitoring and visibility of critical information in real-time.
Digital care management also allows for instant reporting, which gives managers back their time to ‘walk the floor’ and interact with their staff and clients.
Megan Read, Care Home Manager of Grassington House emphasises how the digital system has improved her ability to manage: “Because I have a digital overview of real-time information I can easily monitor what is happening within the home. I can set up anything I want to be recorded, schedule things for the carers to be aware of and make sure that nothing is getting missed.
“For when I’m conducting care plan reviews, I can look at the logs that carers input to directly review and evidence any changes made. Beforehand, you would have had to look through endless files and pages, and you simply wouldn’t be able to go through it all. Now, I have no files in the office, everything is on the system; my office can literally move around with me anywhere.”
Simon agreed: “In leadership, the digital system is allowing managers to spot issues more quickly; alerts raised by carers come straight through to the manager, who can then respond quickly and with all the necessary information”.
Paul added: “Monitoring the quality of the support provided is much more efficient and less intrusive; utilising the Cloud to view live records. It is easier to ensure care is being given and support is provided how the individual would like to receive it. Teams are now positively communicating and sharing ideas, and where changes are required, managers can make these instantly, either across the organisation or simply for individual.”
Managers can also easily establish what information they want recorded, and monitor whether this is being followed. Megan states: “As a manager I can literally prompt what information I want recorded from carers and when. The amount of detail I can now see in recorded notes is amazing compared to what it used to be on paper.”
Simon has also experienced improved quality of care information: “During the transfer to digital care management, we’ve been able to see the quality of our care plans. It is an impossible feat to trail through reams of paper plans for every single resident, but with digital we can check care plans easily and demand the quality we want. It’s meant we can really see the overall process and make sure the right care is being delivered in line with the residents wishes.”
As Simon and Paul state, by recording care as you go, you create a more person-centred and accessible quality of care and you have more time available. Carers have the tools and information they need to provide personal and responsive care, and with extra time, can involve the resident directly and sociably in inputting the care notes.
Megan encourages her carers to be sociable and engage the residents when writing notes; this can mean sitting down with the resident, having a cup of tea and a real conversation about how the resident is doing. She has found that residents prefer the digital care management system once they understand it because carers are able to spend more time with them. Megan commented: “Carers can be sociable and engage with residents so they can contribute to their own notes, keeping them much more involved with their care. Beforehand, carers would have to spend time away from the residents at the end of the shift completing paperwork. The digital system is also really useful for bi-annual reviews; I can hold a meeting in the lounge and connect my laptop to the main screen so we can all see the information and have a really good chat about the care plan with the resident – it’s a lot more involved, but also efficient, and residents like to be able to see their care plans so easily.”
Care information recorded electronically is also much easier to share; not only with other medical professionals, but also with close friends and family. Innovative care providers can utilise existing resources and involve these other parties from the very beginning; you can enable a service user to design their own care plan, involve family members in the on-boarding process or allow informal carers to contribute directly to the care notes. Having a digital system opens up vast opportunities to get better connected with the whole circle of care.
By enabling better communication and ensuring information is shared with those who need to know, your care team will be more aware of the individual service user’s needs; and ultimately, informed care leads to better care.
Get in touch today to see how digital care management can work for you.
Digital transformation in the care sector is no longer the future and the benefits of the technological revolution have been felt far and wide across the sector.
Despite this, and the numerous benefits that technologies have shown in all areas of care, we are still seeing some reluctance towards digital transformation. While there is a common misconception that this is down to many care professionals fearing technology, this is simply not the case.
Past research from Skills for Care revealed that 95% of those working in the sector use digital technology in their work; and that the great majority are strongly positive about the potential of digital technology to improve efficiency and quality of care services. We also know that digital transformations are occurring, because we work with care providers up and down the country who are looking to digitise their care records every day.
It is, therefore, not the fear of technology that acts as the barrier, but, in fact, the fear of change.
In our experience, there is a clear misunderstanding between what the perceived barriers are to adopting technology, versus what the actual barriers are.
Few worry about job automation. There are many instances where advancements in technology remove the need for physical people – you only need to go to your local supermarket to see self-service check-outs, or go online to realise how much of your daily life you can manage without interacting with a person.
In the care sector, however, suggestions that Pepper the Robot will eventually replace carers are disregarded because there are two key things that computers cannot impersonate: social intelligence and emotional interpretation. The adoption of technology in care is not about replacing human interaction, but facilitating more of it through time-saving.
In contrast, the biggest barrier that we do hear care providers talk about is their concern that their staff will not have the necessary skills or inclination to adopt technology. In reality, we actually find the opposite is true.
According to Skills for Care’s The State of the Adult Social Care Sector and Workforce in England, 2017, the average age of a care worker is 43 and a fifth are aged over 55. Data from Statista shows that in these age groups, smartphone ownership is at 88% and 47% respectively. So, the physical use of technology is not alien. With a new younger generation of care workers coming into the sector, all of whom have grown up using technology, confidence in ability is only likely to increase.
The level of notes we have to record in care is often a point of contention and this can also act as a barrier. However, the fact of the matter is that we have to record notes, because without doing so, we have no method of evidencing care. After all, ‘if it wasn’t written down, it didn’t happen’.
It’s not about working out how we can get away with recording less information, but instead how we can improve the amount of high-quality information we record in the least amount of time. This is exactly what digital solutions allow you to do.
Further to this, technology also allows you to make use of all of that recorded information, so that it can be better used to directly benefit care; rather than being filed away in a locked room.
The problem, usually, is not care team capability or the use of the actual technology, but how the digital transformation process is approached, and the tools and support provided during this process.
Going from paper to electronic care notes and care plans is not just a change in the physical process, but also to the content that is recorded. As a result, the approach to managing the change must address culture as much as technology.
In the latest issue of Care Management Matters, our Head of Digital Transformation, Luis Zenha Rela, explains how care providers can implement an effective change management process.
You can read the full article online here.
Digital transformation will never be a ‘one-size-fits-all’ scenario, and the power of technology comes just as much from how it is integrated as the functions of the technology itself.
Embrace this innovation, choose the right solution for you and give special consideration to the change management process, and you might be surprised by how much technology can enhance the quality of care your service provides.
Last week, we attended yet another fantastic Dorset Care Conference, hosted by Care Management Matters at the Lighthouse in Poole. This time, we were invited to present on the role of digital in modern care delivery.
The fact that so many people joined us in the discussion was testament to the event organisers, but also showed that more and more care providers are considering how technology can help them improve the way they plan, record and report care.
Our care consultant, Luis Rela, shared some useful tips on how to approach the digital transformation process and how change management is key; while Juliana Jeffery from Luxury Care Group talked about her experience of using the Nourish system in her care home and how to overcome challenges.
The floor was obviously open for questions at the end, of which there were many. Here, we’ve shared a few of them.
Understandably, a banker in the audience wanted to know about the return on investment of going digital in care. Luis explained that there are both tangible and intangible benefits, and that care providers should think about the bigger picture when considering investing in a digital care management system:
“The tangible benefits are easier to define, of course. You only need to think about the paper you will no longer need to print, store, archive and shred to understand how those costs can be reduced over time.
“There are then intangible benefits such as time saved by recording notes digitally. Many of our care providers say they save at least one hour per carer each day because they don’t have to spend that time at the end of a shift writing notes and instead, record as they go. For some care organisations, this leads to a cut in the number of staff needed on each shift. However, what we find is that care providers instead maintain staff levels to increase the available one-on-one care for residents.
“In fact, one provider said that this decision led to them achieving an outstanding rating with CQC across three of the homes in the group.”
Juliana added: “There is also less time needed to get new or agency staff up to date with individual care plans and they have the time to get to know and spend time with that resident instead.”
So digital transformation is not primarily about driving costs down but improving the amount and quality of care that can be provided.
We were joined in the room by care providers of varying sizes, and many of them wanted to know how much time it takes to go from paper notes and care plans to digital ones.
Luis said: “Typically, it takes two months and we break down the transfer into stages; starting with daily notes and then care plans. However, this really depends on the size of the care home and whether it’s part of a group. If you take Luxury Care for example, they are still going through the process but that’s because they are doing one care home at a time. It also depends on whether we are developing unique features that work with their service. In one instance, a provider wanted to amend the digital care plan template to mirror that of the paper one, so we would do that first.”
Another member of the audience, who is already using Nourish in their care service, commented: “You could argue that there is never an end date once you are using an electronic care management system because you are always evolving and innovating. Every day we are learning something new and get more confident with the system, so every time we have a new idea, we integrate that into our process.”
Going digital obviously involves the use of physical handsets and electronic devices and some members of the audience were concerned that the responsibility of purchasing such equipment would be left to them.
As part of the Nourish service, we provide tablets for managers; handheld devices similar to Smart Phones for carers; and secure log-ins to our cloud-based system which can also be accessed from desktop. The number of devices needed will usually be the same amount of people you will have on each shift. The user will keep the device for the full duration of a shift, log out and handover to the carer taking over the next shift. Each member of the care team has their own log in with set permissions that have been pre-agreed and there are also log ins for agency workers.
Luis explained why this is the best way forward for everyone: “Care providers do not need the added pressure of having to find and purchase their own compatible devices and set them up. Because our software is completely adaptable to the care you provide, we get these ready for you prior to your training. We also have a dedicated technical support team on hand to help you with any queries.”
During her part of the presentation, Juliana explained how having a digital care management system in place had made communication between members of the care teams much easier and members of the audience wanted her to expand on that.
“Because it’s as easy as using Facebook and the device is with them all the time, it’s great for communicating important messages between members of the care team,” said Juliana. “Everyone can see and send messages through Nourish and handovers are now seamless. It’s been brilliant for ensuring everyone is informed immediately. For example, we also use this system to make sure we notify everyone of quality assurance audit results, which would otherwise have been left for meetings. Now everyone feels involved.”
Juliana also highlighted the added benefits of using these devices when recording notes: “We have carers who are not confident in writing notes or perhaps English isn’t their first language, so they love the speech dictation feature. As you speak, it records what you say.”
If you have any questions about the role of digital in modern care delivery and would like to find out how your care service can benefit, please give our team a call on 02380 002288.
As a whole, the care sector is yet to fully embrace the power of Digital Transformation and all of the benefits that can offer.
Working with Care Management Matters magazine, we shared our views on how to make the most of current digital technology within the care environment; to enhance the depth of notes and care plans, to allow a greater degree of control across the management process and ultimately support care providers and care teams to provide the best possible quality of care.
Gaining knowledge and insight from three care providers who have embraced Digital Transformation, the article answers some important questions. How does the digital system impact at the individual level? What impact will the digital system have on staff? And how will that impact the quality of care you provide?
The full article can be found here:
Below, however, we discuss our Five Top Tips for how you, as a care provider, can make the most of Digital Transformation.
Firstly, for a smooth, quick and efficient transition there will need to be strong board-level support to align all stakeholders. One key tip would be to develop an in-house ‘centre of excellence’ team of skilled staff that can focus on digitising and integration.
“To make the most out of electronic management, a provider must be committed to change, with a fully equipped staff team who believe in it” – Paul Dennis-Andrews, Operations Manager (Encompass)
The most successful organisations will be those that gain feedback direct from the care team. Listen to the everyday challenges your care team face. Evaluate and assess how these challenges can be tackled and overcome before you start the move to digital.
“Ensure the staff that will be using the system are also involved in the decision-making and transition. These are the people who will directly use the system and will raise queries or concerns. It has to be inclusive or it just doesn’t work properly” – Simon Francis, IT Project Manager (Silverline)
The transition to digital can be a lengthy process, but it is also an excellent opportunity to review your paperwork templates and quality of care plans. To allow for a smooth transition, it is crucial that you have your current records in order.
“Ensure that before making the transition to digital, your paper records are in good order. This will make the transition a lot smoother and a lot less stressful for your staff. If you are trying to get your paperwork in order at the same time as transition, you will create extra work for your team. You should also identify any differences between your paperwork and how that translates onto a system. If you can make that as close as possible, the transition will be streamlined and much easier for staff” – Simon Francis, IT Project Manager (Silverline)
The best digital care management system needs to be flexible and enhance your care team. It will support the great work your teams are currently doing, rather than forcing them to work in a different way, and it will offer more than simply a digital representation of your current records. Do your research, understand what it is you want from a system, and find a system that matches your needs.
“I work with a system that is responsive, adaptable, instant, consistent, person-centred and surprisingly cost efficient” – Paul Dennis-Andrews, Operations Manager (Encompass)
“We have been able to work directly with our system providers to give feedback and make direct changes; we very much feel like stakeholders in the system” – Simon Francis, IT Project Manager (Silverline)
Finally, if you’re going to transition to digital care management, you need to commit fully. Having some records digital and other paper causes confusion and extra work for staff members. It also undermines all of the benefits of full integration.
“It’s about having all your information in one place, which you simply can’t do on paper. If you’re going to use an electronic system, maximise it to its full potential and move everything over; certificates, audits, training. I have been able to stop writing my endless to-do lists because my system does that for me” – Megan Read
Have you embraced digital transformation? What did your experience teach you and what top tips would you share?
To find out more about how we can support you to make the most of Digital Transformation, please don’t hesitate to give us a call on 023 80 002288.