We recently attended Scottish Care’s Care at Home & Housing Support Conference 2025
The theme ‘Compassion in Crisis’ highlighted the reality of care at home in Scotland today, the opportunities that lie ahead of us and how we can work together to achieve them
The day featured insightful talks, engaging seminars and an intimate opportunity to connect with people from across home care in Scotland
A crucial aspect of several of the conversations in Glasgow addressed the need to view care for what it truly is, a valuable investment that drives economic growth and community wellbeing at a local and national level
Scottish Care’s Chief Executive, Donald Macaskill
Dr Macaskill discusses the focus of the event. He also details the incredible potential of home care. Explaining how care can be good for both society, and the budget.
Scottish Minister for Social Care and Mental Wellbeing, Maree Todd (SNP)
Minister Todd speaks passionately about home care. She draws upon her personal experience in health and care to understand the needs of the sector. Her insight informs her calls to change the perspective of social care from a ‘cost’ to ‘investment’.
Scottish Care’s Technology and Digital Innovation Lead, Nicola Cooper
Explains the importance of responsible AI. And why keeping a ‘human in the loop’ is so important when building AI models.
You can watch other recap videos and read more about Nourish here.
Technology initiated a sea change in social care. The rapid uptake of digital systems in social care saw the number of providers using digital social care records (DSCRs) double in the past four years. This impacts every aspect of the care community, from the processes we use each day, to the outcomes people using support experience. The benefits a provider can enjoy from ‘going digital’ are well documented. What is less well documented is the impact technology, and by recent extension AI, have on our perspective. Specifically, our perspective of ‘what good looks like’ in social care.
We sat down with Lewis Sheldrake, an expert with over 15 year’s experience working in local government and a legacy of innovative implementations of technology and training to discuss this topic. Lewis won the prestigious Local Government Challenge in 2023 with his novel AI Labs project. This project centred on ‘leveraging AI into all aspects of local government service delivery’. Crucially, in a way that supported emotional intelligence and promoted human interaction, two core tenants that ran through our conversation. We chatted about the changing perspectives on what good looks like in social care; moving from reactivity to proactivity, the relationship between data, AI and benchmarking in care and why we need to be open to new opportunities in technology.
Lewis Sheldrake spoke to us in a personal capacity and not on behalf of any local government or association.



“From a local authority point of view the absolute baseline of what good looks like in social care is not having any kind of substantial safeguarding risks. Not being in a position where you’re leaving your most vulnerable without care. Or not essentially fulfilling some of the statutory duties that are placed upon local authorities under the Care Act.
“You can probably already pick up the fact that a lot of what I’m talking about is the absence of certain things happening, as opposed to it being a positive. I think that, unfortunately, is part of the challenge that we face. Looking at this through the lens of local authorities, it’s mainly focussed on avoiding crises, rather than proactive, aspirational care.
“Whereas if you were to put it from the perspective of a person receiving care, it’s different. For them, it’s having that assurance that the care that they are receiving is safe and of a good quality. So they can live safely and independently in their own home for as long as possible
“This contrast in perspective is critical, and it’s exactly the point from which we must evolve. It creates the space for technology to bridge the gap and, crucially, help redefine what ‘good’ can and should look like in modern social care.”



“Firstly, I think it’s important to understand that by the time someone gets to their local authority they are at a certain level of need. Their needs are relatively acute and consequently are going to require a level of intervention. One that’s likely expensive at that stage. This is the reactive model we’ve become accustomed to.
“We often hear cases where a family member can no longer cope. They’ve been providing informal care to that loved one and they’re burned out. Under the Care Act 2014, the local authority has a statutory duty to assess those needs – and where they meet eligibility criteria, arrange appropriate support. By this stage, the intervention is often urgent, complex, and resource-intensive.
“This is happening at a time where councils are absolutely creaking with the volume and complexity of demand that is arriving at their front door. And I think invariably that so many of these cases could have been foreseen with the right technology and data in place.”



“Absolutely, with the right technology we could intervene earlier to help the person avoid requiring a care package for longer. Keeping them there, living well and independently for longer. Supporting their next of kin to be able to continue to provide that care but also have some respite for themselves. I think this is where technology really can fit in. There are two key components of this.
“The first is about being smart in our uses of data. There are some really good examples from my experience around using data. Such as a council utilising data from other interactions it had with people to help build greater levels of prediction. Initiatives to understand when somebody is deteriorating to such an extent that a proactive intervention would be valuable.
“I know during COVID a council were able to identify with 95% accuracy which of their residents would likely be on the shielding list. Through the use of data, they’re able to accurately predict those people and proactively support them. I also know of councils who utilised data to develop predictive falls models. Again, this significantly changes the effectiveness of care, as we can proactively reach out to at-risk people and offer them interventions. Interventions which, along with improving quality of life for citizens, save the local authorities money.
“The second part of this is through digital technology devices. For example, in the case of falls, a device that can detect when a person falls and activate an alarm in response to send for support. But beyond responding to incidents, there’s increasing potential to analyse the patterns and behaviours that often precede a fall. This allows us not just to react, but to intervene earlier or mitigate the risk before a fall occurs at all.”



“I think both of these aspects, if used coherently, will alleviate the amount of pressure arriving at the front door of local authorities. Both in volume and also in terms of acuity. Now, by the time someone is coming to you for a care package you already have a more rounded understanding of their circumstances. Who they are, the context they live in, and the support networks around them. . The volume of that home care they need is less than it otherwise might have been thanks to earlier, preventative interventions.
“In effect, it helps smooth the peaks in demand – reducing the levels of complexity and acuity of cases presenting at any one time. Which in turn lowers the cost to the council and the financial burden on the person receiving support.”
“It’s central. Broadly, there are two ways of using data to understand need and provide effective care.
“There’s the strategic, macro use of aggregated data across large population groups. This approach is highly effective at generating predictive models that assess risk and identify patterns. Providing valuable insights for both providers and commissioners. It enables more intelligent, data informed decisions about how services are designed and delivered, ensuring they are suitably tailored to meet the needs of their clients. We’ve seen examples of this approach applied with great success in other high-risk sectors, such as the aviation industry.
“The second way, and I think the more exciting side, is the micro, hyper personalised application. Where we can focus down on the individual to really understand their needs and ambitions. Again, we see impressive examples of this data application in other sectors. Such as the preference-driven algorithms behind Amazon, Netflix, and Spotify. As well as personalised customer journeys across digital platforms.
“If you were to think about how some of those principles that underlie their architecture. Albeit very different sectors with very different objectives. It raises an important question: what if that architecture were applied to a health and social care context? How helpful that would be to ensure people are getting exactly what they want and need, when they want and need it?
“One of the most powerful aspects of this shift from reactive to proactive care is the ability to anticipate. In social care, hospitals, and communities, we often hear the same phrases: ‘It was only a matter of time.’ ‘We could see this coming.’ These reflections highlight how predictable many crises are – with hindsight. With the right acquisition and application of data, we can change what good looks like in social care in a positive, person led way.”
“If we break down the core functions that exist in care, there are a number of different actors doing different tasks e.g. care planning, initial assessments, delivery of that care. I think there are really compelling applications for AI for each of those. Applications that can enhance the delivery of that function, while in turn delivering a higher level of quality and precision to the end user.
“We’re already seeing promising examples of AI reducing administrative burden with data entry. In terms of things like transcription and data input. I think it’s a good start, but there is significant untapped potential to expand AI’s role across the wider care ecosystem.
“For any care plan that’s pulled together, you think about how many other care plans have gone before that. Drawing upon the decades of experience and knowledge from the people that are inputting into those care plans. With AI this information can be readily triangulated to make the most precise care plan for any given set of circumstances. AI can prompt follow up actions or suggest referrals based on all the data your service has. These prompts support care decisions rather than automate them. Helping to standardise the service offer based on the individual needs of each client, by drawing upon the wealth of experiences and outcomes across your service to inform best practice. Ideally alleviating the variability of individual social workers, while enhancing the specificity of your care plans.
“The data gathered during this care provision is then fed back into the system. This creates a virtuous cycle of person led, community centred care. And that’s just one quick example. From high level strategy to direct care delivery in people’s homes there are applications for data and AI that improve service quality, operational efficiency and ultimately deliver the objectives that keep people living safely and independently in a place they call home for longer.”
“The most immediate answer is reducing administrative burden. There’s lots of opportunities for AI and care technology in general to afford people more time delivering what they got into the job to do. Face to face care, in a more personalised and informed way.



“Let me offer a counterpoint. There’s a common misconception that, more human care always equates to better care. But in some cases, that’s not true. Overprescription and unnecessarily invasive care can diminish a person’s independence and dignity. Take supported living settings for example. Imagine someone with learning disabilities who receives 24/7 care. There are people coming in, waking them up in the night to routinely check in on them. This is well-intentioned, but disruptive. In such cases, the use of technology there can help provide that person with a more respectful and person-centred alternative. Providing greater levels of privacy, independence and dignity. While still ensuring support is available when genuinely needed.
“My key point is about precision and that is certainly where I think AI can play a transformative role. Ensuring care is sufficiently proportionate to the needs of the individual. I don’t think that necessarily means more care is better. I think it’s about the quality, appropriateness and value of the ‘care’ being provided.
“Care in inverted commas mind you, because we’re using care as a kind of umbrella term for a whole number of things at the moment. A lot of responsibilities that are falling under the umbrella of care are not actual direct care. They are different forms of administrative tasks. We need to think about how to displace that through the use of AI and other digital tools to ensure that we are maximising our resources and delivering the best outcomes possible.”
“Absolutely, I think it has too. We have to be realistic. There are massive capacity challenges both in terms of the workforce, and also in terms of the budgets to support social care.
I personally think there are circumstances where technology could well replace some types of care which are not necessary to be delivered in person. With an ageing population and increasing levels of need and vulnerability, we have to use our finite resources wisely. Care capacity is not limitless, and technology offers a valuable opportunity to redeploy human effort where it’s needed most.”
“Understandably so, there are massive capacity challenges in social care, both in terms of workforce and budget. But rather than viewing these constraints purely as limitations. They invite us to re-examine our definition of ‘good’. They imagine how technology and AI can shape what good looks like in social care into a new vision. One that’s more sustainable, personalised, and outcomes focused.
“So much care provision is historically focussed on things like washing, bathing, food, medication. But if we consider this through the lens of Maslow’s hierarchy of needs. These are foundational; they sit at the base of the pyramid. Essential, yes, but not sufficient for a fulfilling life.”
“What it often fails to address, whether due to technical limitations or lack of resource, is anything related to the higher levels of that hierarchy. Support for self-esteem, companionship, and emotional fulfilment is frequently absent. Let alone opportunities for people to self-actualise!
“I really believe that there’s an opportunity to move away from the primary function of care provision being to give people the bare necessities and to basically keep them alive.
“An opportunity for us to move to a form of care that helps people have a greater level of self-esteem, belonging and purpose. Take social isolation for example. Everyone is aware of our social isolation problem and the significance of its health implications. But actual interventions to address this issue are sparse, largely due to cost.
“I think there is huge potential to augment existing models of care using technology and AI to alleviate some of these kinds of challenges.
“AI tools, even just the currently mainstream ones like ChatGPT offer fascinating potential in supporting social connection, stimulation, and engagement. For some people, these platforms provide opportunities to engage in meaningful conversations they might not otherwise have. Interactions that validate their experiences, challenge their thinking, and stimulate them intellectually. It’s obviously not care in the way that we understand and conceptualise care and certainly traditionally. But when you stop to think about it. If someone is able to enjoy an engaging conversation about a subject that’s meaningful to them, that validates their experience, challenges them and stimulates them intellectually, isn’t that a core tenant of ‘good’ care?
“I think there’s value in that. These possibilities have scope, and the potential to progress much further and I don’t think it should be ruled out. Absolutely, AI and technology can help drive more informed decisions, reduce administrative burden and promote coproduction.
“But if we just look to use technology to fulfil functions already fulfilled by traditional models of care. I think that would be a missed opportunity.”
Change, from social care to sofa cushions, is a constant.
For a decade we at Nourish Care have been proud to help shape that change in social care. When we launched Nourish care technology was in its infancy. A vague selection of ideas and applications attempting to address a complex collection of people, processes and promises. Our approach was rooted in our understanding, bringing together our technical expertise with our personal experiences of care to ensure that care technology always put people first. From the very beginning, Nourish has been built on one simple but powerful belief: the person supported matters most.
This belief is why we develop all our functionality through coproduction. Our commitment to collaboration is felt throughout our system. Thanks to this approach our understanding of care is deeper, our experiences wider and our expertise sharper than when we started. We continue to grow with our users just as social care technology enters its awkward adolescence. The past decade has shown us the potential for technology in social care, while Nourish users have revealed to us the best applications for our software, opening our eyes to the opportunities for supporting positive change in the wider system of care. In response, we are releasing several new Nourish products to support the wider care sector.
This expansion of our application is rooted in keeping people at the centre of our systems. We know growth demands structure, scaling demands clarity, and crucially, care demands trust. Structure can be built, clarity provided but trust, trust must be earned.
Nourish Care is the longstanding name of our platform and our business. More than that it is a promise, a commitment to community, coproduction and care. We will be changing the name of our platform to accommodate the new products we have developed for the wider system of care.
We are keeping the promise.
Our new naming convention reflects our renewed focus on people. Technology should feel as natural as the care it supports. That’s why we’ve ensured that every product name reflects not just what the platform does, but how it makes people feel.
Nourish Care will become Nourish Better Care
It’s important to remember where you started! Nourish Better Care is the most trusted and customisable care management system for residential providers in the UK.
Nourish Rostering will become Nourish Empower
All the tools a home care provider needs to support their community and manage their service.
Nourish Community will become Nourish Better Care at Home
Combining the mobility and admin of Nourish Empower with the industry leading point of care functionality of Nourish Better Care to support effective processes and drive improved outcomes.
Nourish Mobile Device Management (MDM) will become Nourish Protect
Keep your devices secure and your community’s data safe with our mobile device management system.
Nourish Insights
Get the full picture of your service with our data dashboards so you can make more informed, more effective decisions.
Nourish eLearning
Available through our home care platforms, Nourish eLearning offers an integrated, accredited by CPD and Skills for Care, library of care courses for your team to utilise, supported with real time reporting.
Nourish Care will continue to be the name of our business, with the specific names of products reflecting the impact they deliver for care providers and your communities.
We are not the only ones changing. You are too. Our users have changed so much over the past decade, through digitisation, updated regulations, and new legislation, without ever losing sight of the people that make care so special. With our new, multiple product approach, we are establishing our foundation for future growth alongside you. So, we can best respond to the needs of today, and the challenges of tomorrow.
No two people with support are the same. Uniqueness is the blessing, and the curse of social care. One size will very much not fit all. You need the right tools for the job, and the best people behind them to support you.
To make it easier to find the right products for your community we created the Nourish Product Ecosystem. Each circle reflects a different focus for our products and the impact it will have on your community.
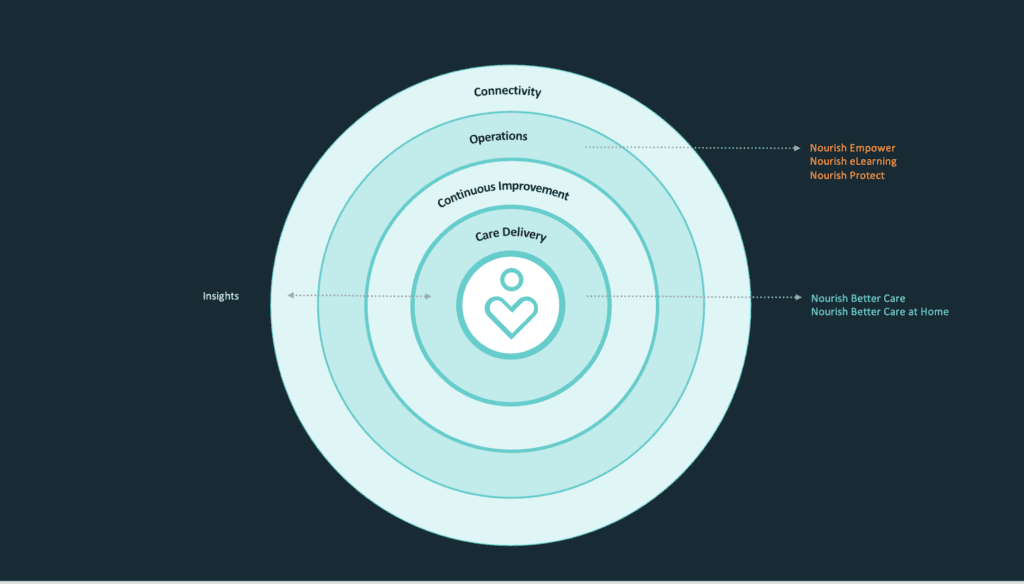
Care Delivery – For Feeling Supported
Technology that steps back, so care can step forward.
Continuous Improvement – For Feeling Assured
Because confident carers create safer, more consistent outcomes.
Operations – For Feeling Secure
Supporting care teams to be prepared, skilled, and sure of what comes next.
Connectivity – For Feeling Connected
Bringing together every piece of the care puzzle around the person.
This approach goes beyond categorisation. It lays the foundation from which every new product, every innovation, and every solution we launch builds towards something bigger.
Most importantly, it ensures that as we scale, we never lose sight of what made us great, keeping the person supported at the centre of care.
Imagine a healthcare system where care teams feel empowered instead of overwhelmed. Where families feel reassured instead of disconnected. Where people receiving care feel safe, valued, and heard.
That’s the world we’re building.
And we’re not waiting.
We have coordinated internally
So our teams live and breathe this philosophy.
We are communicating externally
So our customers feel the impact as soon as possible.
We will continue to co-produce
Because technology should evolve with the people it serves.
Change is a constant, a promise, and a challenge. One that can only be met in the same way we always have here at Nourish, by working together. Coproducing our products so that people are always at the centre of everything we design, develop and do. Because after all, change, like care, is human.
We’ve got lots of exciting plans coming soon, if you want to build the future of social care with Nourish, contact us directly today.

The future of social care in the UK is linked to the future of the NHS. One cannot progress without the other. So, when the NHS established the Assured Solutions List (ASL) to help shape the future of digital social care, every software supplier in the sector took notice. NHS Assurance is a clear badge of quality and ambition. Nourish Care was the first Digital Social Care Record (DSCR) to join the ASL. A statement of our commitment to both compliance and innovation in care technology.
The purpose of the ASL is to encourage care providers to digitise. By establishing a trusted baseline of system requirements and providing funding to help providers get started. The requirements for membership of the ASL granted confidence to providers of the capabilities of the system they were using to digitise their processes. NHS Assurance guarantees safety, security and reliability for care providers when choosing their digital partner.
Since Nourish joined the ASL, it continues to expand in membership and calibre. This year saw an expansion of standards with the introduction of 14 new standards. These standards built upon the baseline of requirements for assured solutions and indicated the coming ambitions for health and social care interoperability. They covered a range of important issues, including the use of data, information sharing, security and integrations.
It is crucial to use a system that complies with these standards to set yourself up for the future. Most suppliers are still yet to be approved on all 14 standards, you can see how far along they are here. Click on the supplier and navigate to their ‘Standards’ drop down.
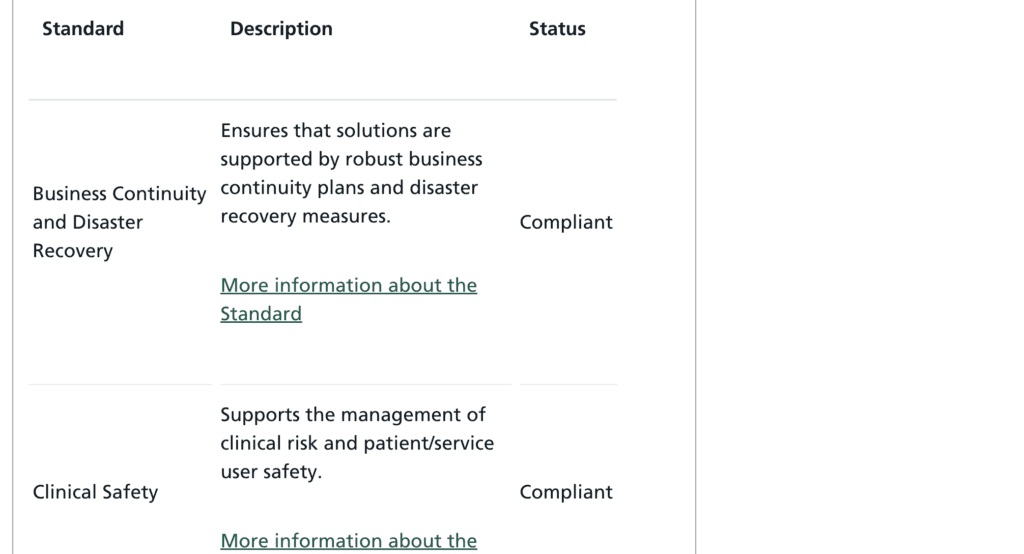
It is clear the NHS have further designs for the ASL and its members. Compliance with the existing standards indicates a supplier is aligned with the future direction of digital social care. When looking to your own future it is important to ask the suppliers you utilise about theirs.
What connections do they have to the NHS?
What is their approach to interoperability?
How committed are they to maintaining their standards of compliance and information security?
Ensuring alignment with your digital supplier is vital for building a future-proof and secure business. Ensuring your system and service are qualified with NHS assurance. If you are curious about switching your digital system to a new supplier, we have prepared a useful document detailing the process with us. You can view it here.
If you would like to learn more about how Nourish works with our users to wrap our system around your service, you can read our case studies here.
One of the clearest requirements of the new 14 standards for NHS Assurance is interoperability. The ability to record, store and share information securely. This is in direct response to the ‘sin of silos’ that plagued health and care providers for decades.
Along with our adherence to these standards Nourish also champions interoperability through the Nourish Partnership Programme. This initiative reflects our commitment to building solutions across suppliers to best serve care providers and their communities. We are proud to develop social care led solutions alongside suppliers, providers and our wider communities.
The NHS and social care move together. In September Wes Streeting announced ‘three key shifts’ for the NHS. With recent developments for the ASL, increased focus on compliance and a commitment to interoperability it is obvious this shift is coming to care as well. We previously explored the move from ‘Analogue to Digital’ here. The ability to deliver the other two key shifts, namely ‘sickness to prevention’ and ‘hospital to community’ will largely be defined by the ability of different health and care providers to share their information with each other. The ‘Data Use and Access Bill‘ highlights this focus from the UK government and points to the significance of membership to the ASL for digital social care records as a baseline.
It is clear digital systems will play a huge role in the future of health and care in the UK. Now is the time to make sure you have a partner you trust, understand and enjoy working with.
Now is the time to talk to Nourish, because things are just getting started.
Compliance is crucial for home care providers. Evidencing compliance is vital for care providers meeting regulations and ensuring compliance is important for providers delivering quality care. Whatever form your regulator takes, or whatever reforms they implement, it is vital you can tell your care story. Home care compliance is particularly important due to the incredibly personal nature of welcoming a carer into your house. It requires a feat of great trust on the part of your customers. A trust that is sacred to the quality of care you provide and the standard of your reputation. Any home care business looking to grow and secure new customers needs to be able to tell their care story effectively. One that shows your compliance with established regulations and ability to support your community.
The right digital partner can help you capture your care stories and share them with all your stakeholders. This can go beyond your regulator, to your wider circles of care and community. All relationships are defined by the trust you share with each party. Nourish Care gives care providers the tools to capture all the information you need, understand it on both a micro and macro level, and build case studies that show the quality of your care.
It is vital you capture the right information to tell your care story from your care delivery. Everyday thousands of small acts of personal empowerment are provided through home care. Don’t sell yourself short by letting them slip through your forms! With the right digital care management system you can rest assured your team is recording everything you need.
Nourish Care records all the information from your team in real time through our app. This simplifies the process of recording, and subsequently reporting, the care you provide. Helping you to tell an accurate care story to your regulator. Home care compliance is further boosted through the audit trail capabilities of our system. This charts all actions on the Nourish platform, giving you a clear timeline of activities. Which in turn ensures care delivered can be easily evaluated to promote quality as well as the right care being delivered to meet people’s needs, wishes and preferences.
This is particularly important for home care providers who need to report actual appointment times. We offer a selection of call monitoring options, including devices and a start/stop button on our app. This guarantees a wealth of information for your coordinator. Information including the actual appointment times and the location of the sign in, as well as capturing all of the relevant interactions that occur during the appointment.
Each of the interactions captured during an appointment constitutes a data point. What they ate, when they ate, what exercises they did, where they went, what they drank, how they felt. Nourish automatically plots these data points for you, weaving a tapestry of information on your care delivery for you to share.
You can use the information Nourish presents you with to identify trends. Trends that unlock a deeper understanding of your care for everyone involved with your service. Your coordinators will be able to comprehend the nature of your care on a range of levels. This provides valuable oversight whether you are a small family-run business or operating as a franchise!
Crucially, it makes it simpler for you to be able to chart and detail your care for your inspector. Show how you engage, understand and respond to the needs of your community over time. A comprehensive, and comprehensible, overview of your service sets the scene perfectly for the nature of your care. Allowing you to then guide your inspector through specific examples and case studies to acquaint them with the day-to-day reality of your care.
Case studies are one of the clearest ways to inform people about your approach to care. We have several of them ourselves we’d love you to check out!
Care is not a static undertaking. Living the life you want is about having the freedom to pursue your interests. Quality home care supports people to do just that. Quality home care software supports providers to record, review and report their life-changing care.
Nourish gives you the tools to build case studies of the people utilising your service. These case studies detail on a one-to-one level of how you wrap your service around your clients. Demonstrate the unique way you provide care to your community, illustrating how you involve people with support and their circles of care. Document appointments and demonstrate how you respond to your client’s needs as they evolve and develop thanks to your support.
Our robust home care app makes involving people in their care decisions simple. Voice-to-text technology and note-taking capabilities means your carers can engage directly with your client’s experiences and record them in Nourish. Showing the person-led approach to care that is championed by regulators across the UK and Ireland.
Home care compliance is more than a box-ticking exercise. It is an opportunity for you to share the incredible care you provide. Too often the true depth of care goes unacknowledged during an inspection. With the right digital home care software you can ensure that every aspect of your outstanding approach is captured.
Regulations will continue to grow and adapt with time, just as will your service and the communities you support. That’s why it is vital you can tell your care story, utilising home care software you trust.
We must crawl, walk and then run. However, as many new home care providers know, there’s plenty to trip over on the way to full speed. The journey from start to Outstanding is filled with unique home care challenges. But with the right people, and the right systems, you can face anything. After all, success is a marathon not a sprint. When you look to your future make sure you think long term. Smart investments early in your journey can help save you time, money and hassle as your business expands.
We’ve put together a list of the 10 most common home care challenges faced by new home care providers with that in mind. Hopefully it can give you a little guidance when you need it.
If you would like to talk to us directly about starting your home care journey off strong, contact us here.
Recruitment and retention are longstanding home care challenges. In Skills for Care’s 2024 State of Care Report there was a vacancy rate of 8.3% in social care jobs. 3 times higher than the national average.
Addressing recruitment is often a matter of retention. Providing your team with a quality work environment, good conditions and understanding is essential. Investing in your people is as important as investing in your technology. You can create a rising tide of care quality with training, engagement and advancement opportunities for your team.
Technology can make managing and championing your teams more straightforward too. Whether utilising time off functionality to simplify rostering or eLearning to make developing your skills straightforward for your team.
Compliance is often intimidating for new home care providers. Getting the information right for your regulator is crucial. You need to be able to tell comprehensive care stories regardless of the imperial initialism haunting your dreams.
Care management systems support home care providers to do this by recording everything you need in one central location. So, you can not only record, but also review and report your data, for your regulator. This empowers you to tell your care story, and get the rating you deserve.
We talk in more detail about the importance of compliance in home care here.
Home care technology offers home care providers the opportunity to ‘future proof’ their business. But what does this increasingly popular buzzword actually mean?
The right software can help simplify your processes. More than this, it can be used to establish your best practice in an easily replicable, and scalable way. Allowing for simpler onboarding of both new carers and people utilising care.
A common challenge for home care providers is poor communication and information sharing. Your carers are experts in their experiences. Home care software helps providers to share this expertise and experience across your whole community.
This includes improving communication with third parties like Local authorities and healthcare services, as well as internally. In the past poor information sharing and ‘information silos’ led to duplication of effort and inconsistent care.
Care technology addresses this challenge by simplifying the centralisation your information and making it easier to action.
Maintaining a high standard of care in a home setting can be challenging due to limited resources and oversight. Home care technology offers a range of solutions to address this. The best of which are fully compliant with the digital social care records standards and are listed on the Assured Solutions List. Best practice can be enshrined in your processes and ensured through your system set up.
Functionality like remote monitoring and warnings help providers to shape and share their best practice across their service. A system like Nourish Care supports home care providers to establish their approach to care, record and review their care application, and continually improve it in line with feedback from their community.
Home care is unique in many ways. At the core of this approach to care is the nature of appointments. Home carers appreciate the sanctity of someone’s home. Home care providers appreciate the sanctity of someone’s schedule.
Call monitoring enables carers to record their actual appointment times. Guaranteeing accurate times and locations for appointment starts. This information is vital for reporting to commissioning bodies. It is also useful for feeding back into your own processes to refine and perfect the flow of your carers through your community.
A schedule is never straightforward in home care. Abrupt changes and unforeseen adjustments are par for the course. Navigating these home care challenges on paper or a digital spreadsheet is incredibly difficult.
Digital rostering simplifies every step of this process. From set up to rescheduling and reporting, drag and drop rostering systems make adjusting rotas simple. Nourish Care boasts a ‘Recommend’ feature that gathers all the relevant information you have on your carers, including travel time, skills and previous relationship with the person drawing on support.
Ensuring that whatever spot you’re in, you can make an informed decision.
Carer burnout is a serious and understandable concern for home care providers. Home care workers can experience stress, emotional fatigue, and physical exhaustion while carrying out their responsibilities.
As we mentioned in the Recruitment and Retention section, understanding is essential. Digital systems can promote this understanding with communication tools, personal development support and better oversight.
Balancing costs, invoices and timesheets can be overwhelming. Especially for home care providers who are just starting out.
There are a number of digital systems that can help you simplify this process. Nourish for home care offers a finance management suite so you can manage payments, organise payroll, and create invoices. We also offer an integration with Sage.
Centralising your financial processes simplifies their management. It can also help you gain a clearer oversight of your finances and help you make more informed decisions about your future direction.
Client acquisition will always be a concern for home care providers when starting out. How do you make sure you are attracting enough clients to maintain your business?
Well, addressing the above home care challenges is a great place to start!
Digital systems give you better oversight of your care, promoting a deeper understanding of your community and driving improved outcomes for the people who draw on your support. Which will naturally spread the word of your care quality across private buyers and public commissioners alike.
So, you can build the future you want for your team, your business, and your community, at a pace that suits you.
If you’d like to learn more about building for your future with Nourish as your digital partner, contact us.
Conversation is crucial in care. Our understanding is built on our ability to listen. Everyone who provides care is well aware of this dynamic. A lesson we learned over the past ten years by working with our users to improve processes, functionality and outcomes. We are creating our Care Voice Champions to ensure we continue to keep you close to our development process.
Too often in technology, we have a ‘story in our back pocket’. An experience someone shared with us when we first started developing software solutions. This story is a great starting point, but it can become stale over time. As a result, developers find themselves working closely to the memory of a challenge, rather than the reality.
Take care notes as an example. The original challenge was digitising a longstanding paper process. The story of carers filling bursting filing cabinets with lonely notebooks echoed in every developer’s ears. This led to several innovations, such as digitising the note-taking process, improving the quality of information available, and making notes easier to review. However, if we stopped talking at this point the innovations would stop too. Thanks to ongoing conversations we developed more specific functionality, like dictation to make recording notes easier, triggers to encourage note-taking at specific times and reporting suites to present the information gathered in more digestible and informative ways.
We created our Care Voice Champions to keep the conversation going.
At the start, we plan to communicate monthly. We will review the effectiveness of this approach and adjust the time frame as necessary. Crucially, it will be entirely up to members of the Care Voice Champions group to engage with a specific topic. We do not require or expect every member of the group to engage on every topic. We appreciate how limited care provider’s time is, and we will make sure this process is swift and simple. Starting out, engagement will primarily be conducted through surveys.
There may be times when we want to have a direct conversation with certain members. These will be requested formally, and well in advance to ensure minimal disruption to your schedule.
The ultimate goal is to build a continuous cycle of engagement and through that strong collaborative links with our Care Voice Champions. We want to make sure that everyone is involved in our journey as a product. We need to understand how you approach care, how our system supports your approach, and how we can work together to drive better outcomes for everyone involved.
We know this will not be an easy process. Indeed, we anticipate a few stumbles along the way. That is why it is so important to us to involve you in the process. Stumbling is a natural part of moving forward, just as honest conversations are an essential part of growth.
If you want to have a more direct hand in our growth, please, join Care Voice Champions.
When Wes Streeting announced his three key shifts for the National Health Service (NHS) at the Labour Party Conference at the end of September social care’s ears were burning. A move from analogue to digital, hospital to community and sickness to prevention is a move towards care. Clearly social care has a big part to play in the future of the NHS. And technology plays a crucial role in the future of social care. When applied correctly digital solutions empower us to improve both efficiency and outcomes. Which offers care technology a central role in the government’s ongoing attempts to stage a digital revolution in health and care. We all know the why, given social care’s enduring challenges. It is uncovering the precise, who, what, when, and how of the matter that remains something of a mystery.
We recently headline sponsored the Home Care Association (HCA)’s Tech & Homecare conference. A day of insights, inquisition and understanding for leading home care providers and technology suppliers. On the day our CMO, Lee Gilbert, hosted a panel featuring a who’s who of digital rostering and AI suppliers discussing data, while The King’s Fund’s Pritesh Mistry joined HCA’s CEO Dr Jane Townson OBE to ask, ‘How can technology solutions help move care closer to home?’. The latter a conversation underpinned by the recently published, Nourish Care sponsored, study exploring ‘The reality of, and potential for, digitally enabled care in the community’. Reflecting the collaborative spirit of co-development that defines modern, outstanding care, these conversations detailed a variety of ongoing efforts to move social care from analogue to digital. Their success, their missteps, and the road still ahead.
Chair: Lee Gilbert, CMO, Nourish
Nuno Almeida, CEO, Nourish
Steve Sawyer, Managing Director, Access Group
Robin Batchelor, CEO, everyLife Technologies
Matthew Bond, CEO, Borderless
Abeed Mohammed, Co-founder, Birdie

There is already a wealth of positive examples of technology improving care quality. Providers applied digital solutions to a selection of the challenges they face. Both The King’s Fund research, and each of the panellists, presented their own positive instances. Pritesh detailed several different, key, areas that are already befitting from digital solutions, such as communication, care co-ordination and personalisation. Dr Townson added to this during their conversation, highlighting some Local Authority’s recent adoption of ‘magic notes’ as an example of technology changing people’s lives.
The panel built upon these cases with a specific focus on utilising existing data in systems. Matt Bond shared how Borderless share and aggregate data to pass benefits to individual people by finding the gaps in your existing service. The other four panellists all pointed to the efficiency their respective rostering platforms bring to care providers. When Robin Batchelor brought attention to the current inflection point in care technology it resonated around the room. Nuno Almeida agreed, “We’ve spent 14 years building the foundations. It’s not rocket science; the rocket science lies in your ability to react to needs.”
That is the crux of the matter, when we move from analogue to digital, we have to retain our focus on people’s needs. The ability to react to these needs is defined by our ability to engage with them. One of the biggest fears about moving from analogue to digital is based in the apprehension of losing the human touch that has always guided health and care in the UK. A fact reflected in two of the recommendations from the King’s Fund’s research. The need to ‘Shift culture to embrace the public’s digital capability’ and ‘Support staff to embed tech in their roles’. Neither of which are groundbreaking discoveries, but do require fresh ideas to address. Such as Scottish Care’s Care Technologist role. We know the potential of carers, their adaptability and commitment to any idea that can improve outcomes for their community.



What we need to do is make engaging with, and championing, care technology a simpler process. Which is not something that can be done overnight. “Asking people what is important to them is the biggest gap in our data,” admitted Nuno during the panel. “But this is also a big opportunity for us, asking, ‘What will really make a difference?’” The more we can involve people in the design process, the more ‘frontline’ feedback we can apply to our development. This co-production keeps people at the heart of care technology, which is crucial as we move to put technology at the heart of care.



Dr Townson concisely summarised this issue during her talk with Pritesh. ‘Technology for technology’s sake is not progress’. Innovation cannot be disruption in care, the standard approach for technology entering a new sector. The responsibilities are too great. We have to understand the barriers and develop enablers for adoption in the workforce and communities they support. Any one software solution aiming to promote wrap around care and support needs to ask itself a simple question. ‘How will the care providers work alongside our tech?’

Pritesh highlighted the need for this focus in his research with The King’s Fund. One of the recommendations from this research underlines the need to ‘develop strategies for co-developing digitally enabled services’. Specifically raising the point that developing a strategy for co-development and patient-led service design will help to direct digital service development and strategy. While this suggestion calls for action from ICSs, ICPs, the NHS and the Department of Health and Social Care (DHSC), it speaks to all digital suppliers and providers in social care. The move from analogue to digital in care must involve people at every step, or it is sure to get lost.
Nuno spoke about the need to ‘crawl, walk, then run, to get to data quality’. A process that rings true for all forms of digital technology. When The King’s Fund recommends ‘A national vision to guide local decisions’ it is not calling for a direct mandate. It is asking for a personalisable framework. ‘A guiding national vision, with local flexibility as to how it is achieved. One that will help to align the efforts of technology innovators, health and care providers, and leaders designing improved community-based services.’
The HCA’s conference was an example of just that endeavour. A selection of leaders, creators and providers sharing experiences and ambitions to help shape the future of care as we move from analogue to digital. One based in the commitment to collaboration that makes care the beating heart of our communities. After all, if you’re going to solve a mystery machine, it’s best to do it with a gang.
Scottish Care’s Care Home Conference is a highlight of the social care calendar north of the wall. Caledonian Carers from across the country congregate in Glasgow to share experiences, insights and ambitions. The day features engaging talks from political and care leaders, as well as interactive workshops and an incredible awards show. We must understand and engage with care providers across the UK, and we cherished the opportunity to meet so many shining examples of Scotland’s care sector.
The Glasgow Hilton quickly filled with a buzz of excitement around the ballroom and exhibition halls. We set out our humble stall and welcomed guests from across Scotland. Care takes a myriad of forms, shaped by the people, communities and cultures in which each service is based. We know there is no better way to understand your experiences than engaging with providers directly. The opportunity to meet so many Scottish carers was crucial to ensuring we continue to support them as effectively as possible. Additionally, as we were positioned next to the main speaking area, we had front-row seats for the major discussions of the day.

The first talk of the Care Home Show was perhaps the most heated. An ideal way to banish the cold November morning from our bones. Four representatives from Scotland’s leading political parties shared the stage to discuss the state of social care in Scotland.
The Scottish National Party’s Cabinet Secretary for Health & Social Care, Neil Gray MSP
Deputy Leader of the Scottish Labour Party Dame, Jackie Baillie MSP
Scottish Conservative’s Shadow Minister for Environment, Biodiversity and Land Reform, Brian Whittle MSP
Scottish Greens‘ Spokesperson for Health and Social Care, Gillian Mackay MSP

The crux of this conversation was the proposed National Care Service. An undertaking further down the production line than that of Labour’s proposal in Westminster. The Scottish government recently paused their plans for the National Care Service. So they could review their current plans and make sure they have the right proposals lined up for next year. Neil Gray remains ‘absolutely committed’ to the plan and points to the recent ‘progress over austerity’ approach the SNP are championing.
Several pressing issues were raised by the panel. Brian Whittle pointed to the growing number of ‘care homes being swallowed by councils’. Gillian Mackay built upon this assertion when she spoke about the ‘smaller care homes in trouble’ across Scotland. An issue exasperated by inflation; inflation Gillian attributed to the previous decisions of the Conservative government under Liz Truss. Dame Baillie spoke of the ambition of the National Care Service proposals of Labour’s Westminster manifesto and how they align and relate to the current Scottish plan.
Following a brief Q&A Neil Gray drew the conversation to a close highlighting the challenges of ‘trying to tackle service variance’. Something we can appreciate as learning more about the unique Scottish services is what brought us to Glasgow too. Throughout the panel the politicians were quick to talk about responsibility and slow to acknowledge their respective parties’ contributions to the current state of care. However, there was a denominating understanding. All representatives pointed to the need to treat carers with respect. As well as the need for a renewed focus on ‘the true cost of care’. While the future remains uncertain, you can be sure Scottish Care will do everything in their power to be a part of shaping it.
The next portion of the day involved a series of workshops. These were designed to help attendees learn about a specific point of interest to them. Interactivity was king as the lively conversations spilled out from their respective rooms and into the lunch area. We attended ‘Building Confidence in Digital and Data for Care Homes’. Nicola Cooper, Scottish Care’s Technology and Digital Innovation Lead, and Cheryl Stevenson, Care Technologist, led the session.
Everyone in the room shared their experiences with digitisation. Most providers felt they are ‘quite far along in their process but not excelling’. A common challenge of upskilling effectively emerged. Time, cost and resources for digitising workforces are hard to find. In response, Nicola Cooper spoke about the digital and data compatibility framework Scottish Care are developing. Cheryl Stevenson built upon this point when she detailed some aspects of her Care Technologist role. Including their monthly cyber security meetings. Finally, the session drew to a close with a discussion on the digital health and care leadership programme, and how attendees can get involved.

The afternoon talks covered some more specific issues facing care providers. Although before they took to the stage Weekday Wow Factor addressed the challenge facing the attendees, the post-lunch slump. They hosted a rousing dance party as their members led the hall through some pop classics. We all got moving and were well-energised for the afternoon speakers.
Professor Lesley Palmer, Professor of Ageing and Dementia Design, Stirling University, led a session on the importance of architecture in care home design. Tommy Whitelaw, National Lead Person Centred Voices, Alliance Scotland, followed after. His uplifting session highlighted the ways we can come together as a sector, and the humans at the centre and in the driving seat of transformative social care.
The last talk of the day was led by Scottish Care’s CEO and Deputy CEO Dr Donald Macaskill and Karen Hedge. They outlined their recently launched 5 year plan for social care. They outlined ‘the four V’s’ of their plan, that social care should be Visible, Viable, Valued and Visionary. An inspiring invitation to join Scottish Care as they build towards the future. A future underpinned by the understanding that ‘you [Care Providers] are not in the business of maintaining people, you are in the business of enabling people to flourish’. Helping people to flourish is what we do best here at Nourish, so we were immediately on board!
We left the venue shortly thereafter to prepare for the awards show. An evening of celebrations and shaking tail feathers marshalled by the inimitable Michelle McManus. It was a wonderful time. We are especially grateful to our friends from Care Concern Group and Community Integrated Care who joined us.
The atmosphere was one of elevation. Every nominee took to the stage to raptuous, and well deserved, applause. We want to extend our heartfelt congratulations to all of the nominees and winners, including our friends from HC-One and Priory Group.

We thoroughly enjoyed our time up in Scotland. The Care Home Conference and the Awards were incredible experiences. To see so much joy, pride and dedication in person is always inspiring. Many plans were made for the future of social care, and thanks to the stars we found to follow, we won’t be going agley any time soon.
Growth is a winding road. In October 2023 Nourish Care acquired CarePlanner Home Care Software. The merger brought together two leading social care software solutions for care homes and home care respectively. More than this, it brought together two teams who already shared a philosophy for collaborative software development, and a passion for supporting care providers on their digital journey. Over the past year we combined experiences, shared perspectives and continued to develop best in class functionality for our users, alongside our users, to drive better outcomes for everyone involved.
To celebrate an incredible 12 months, we caught up with some of the old guard from CarePlanner. We discussed the past year, what they’ve been up to, and why they’re excited for what’s still to come.



Combining two companies is a large, but delicate process. One that requires balancing different teams, responsibilities and skills with new opportunities and ambitions. CarePlanner’s Operations Director, now Nourish’s Director of Operational Excellence, Mark Gutteridge was instrumental throughout this transition.
“I oversaw the nuts and bolts side of bringing the two businesses together,” explained Mark. “Things like the processes, the way we work, the policies, making sure everything was aligned. That was the first six months. Since March of this year, my team are responsible for streamlining processes, putting in place new systems, and helping the business remain efficient as we continue to grow and onboard new customers.
“It was a big undertaking, and our guiding philosophy throughout was making sure we always asked the question ‘Why?’. It was a key case of prioritizing what was important and what would make a difference to our users. We brought the two companies together so we would both be stronger. We really wanted to deliver on that potential.
“There’s always a teething period with substantial changes like this. But once things settled down the benefits became obvious. We used to say to ourselves that CarePlanner wanted to do a lot of things, but they didn’t always happen as swiftly as we’d like. When you look at how swiftly we’re launching new features like our eLearning solution now it’s inspiring. We’re able to respond much more quickly and effectively to our users and their experiences. I think that it’s been crucial in terms of making sure we continue to support our users and provide a market-leading product and service. Which is a really exciting place to be.”
Understanding is central to building anything effectively. At Nourish and CarePlanner Home Care Software that understanding has always come from our users. Both companies boast team members with care experience. The combination of our Product teams, along with some experienced new leadership joining the fold, sharpened our focus, while at the same time unlocking whole new ideas to explore.
“The new structure builds upon our established user led approach with a wealth of experience and clinical expertise,” explained Product Manager Robert Baker. “Their focus on the clinical safety and the clinical side of the product is invaluable. It empowers us to understand the best practice around our software so we can shape our functionality to best respond to our user’s needs. We always want to stay as close to the lived experience of care as possible. Because it helps us tailor Nourish to the specific needs and use cases, some of which we’d never discover on our own!
“Fundamentally, the new structure keeps us focused on outcomes. Our attention is firmly on the problems we need to solve. Our teams have the resources and autonomy to respond to customer’s needs in a way that was previously unattainable. This means we can focus on developments for all sides of the Nourish platform, and any of the care types we support, with established care contacts and personal experience to guide us.”



Product teams focused on how to capitalise on our future opportunities to improve outcomes for our users. However, there remained the sizable task of bringing together the functionality the two companies already built for their respective platforms. We spoke to Lead Developer Martin Joiner about how they addressed this undertaking, and the benefits of bringing fresh eyes and open minds to old challenges.
“When we first joined together we were faced with two pieces of software with a lot of unique functionality,” explained Martin. CarePlanner’s home care software and Nourish’s residential. So, it was important to find the denominators. There are a lot of similarities between the systems as well. Features repeated across many platforms like: What does a profile look like? What information does it contain? How is an address formatted? General architecture like that. Lining these points up is a lot of work, but it is vital. We took small steps, one at a time to ensure we aligned the systems closely while still retaining the strengths of the previous structures.
“Of course, just like in care, the real strength came from our people. With so many new people to talk to and work with there are so many opportunities to share best practice. We can ask ‘Why?’ whenever our curiosity is peaked and learn from each other. There are few things better for a problem than fresh eyes and informed opinions. We all value understanding why we are building something. And this close relationship with the purpose of our development process is reflected throughout Nourish’s tech teams. Another key denominator that has shaped our success over the past year. Leading to new developments like TARS, Time Off and eLearning for Nourish home care users.”
Even on the technical level we find ourselves coming back to the importance of aligning on a human one. Personal connections define us all, especially when it comes to building productive, collaborative relationships in every aspect of our business. A maxim held true in both Nourish and CarePlanner.
CarePlanner Home Care Software may have been the industry standard for rostering technology. However, its reputation was built on more than technology, it was built on relationships. Nourish shares that focus on personal connections. A prerequisite requirement for the merger, and a substantial relief to the customer-facing teams on both sides of the acquisition.
“As Account Managers our first focus is always on the customers,” said Head of Account Managers Lauren Ware. “We build close connections with our customers because all Account Managers have dedicated accounts they work with. It delighted us to learn Nourish has the same approach. Thanks to the resources Nourish brings to bear on sector challenges our functionality and integrations have gone from strength to strength over the past year. This empowers Account Managers to unlock new opportunities for our users, and address long-standing challenges.
“It’s one thing to be told your philosophy aligns with another company, it’s a different thing to see it for yourself. Care is a fundamentally human undertaking. For all the changes the sector and we experienced over the past few years, that remains the constant. In Nourish we found partners who share that focus, and the results speak for themselves.”
The driving impetus of the acquisition was to make both solutions stronger. A combination of experience and insight to drive positive outcomes internally and externally for both businesses. One of the biggest changes this caused was for our support teams, whom we combined and specialised to best respond to our users in a timely and effective fashion.
“Bringing together the best of both Nourish and CarePlanner Support teams has been an exciting journey,” detailed Head of Technical Support Cian Connolly. “One that has strengthened our focus on what matters most, our customers. Over time, as the dust of the merger settled, we came to understand the needs of users and the strengths of our colleagues. This inspired us to develop two teams, Customer Support and Technical Support.
“With the move to dedicated Customer Support and Technical Support teams, we’re positioned to provide faster, more tailored solutions. Ensuring every interaction is both meaningful and effective. I’m incredibly proud of our team’s commitment and am excited for the future as we continue to raise the bar for customer experience in care technology!”
CarePlanner Home Care Software belongs to the past. But the people, platform and purpose that shaped it for over a decade remain in place. Committed to the same goals, and the same communities to whom we have always owed allegiance. Nourish is now the largest supplier of social care software solutions in the UK. With over 400k people supported through Nourish and 350k carers driving positive outcomes for their communities every day. A responsibility we all take great pride and purpose in.
The future remains an open horizon, and we have some fantastic company, and a stellar company, to join us on the journey.