


Birthdays are a natural cause for reflection. As Nourish Care celebrate our 10th we find ourselves looking to both the future and the past to better understand where we are today. For 10 years, ever since we got our first customer, Nourish has been proudly supporting care providers across the UK and beyond.
Growing alongside our users, increasing the functionality of our platform and expanding the range of care types we work with. Throughout this journey we remain connected by a singular focus, a golden thread that runs through every iteration and evolution of Nourish. The idea that the people who receive care come first. This commitment to care and foundation in coproduction defines our past and decides our future. As we look forward to a litany of possibilities, from data and AI, to family connections and institutional integrations, it is our focus on people that matters most. As is tradition.



Okay, technically, we are actually closer to 14 than we are to 10. The seed for Nourish was first planted in 2011. This seed of an idea would spend four years flowering into the first iteration of Nourish that was officially launched with our first customers in 2015. These four years laid the groundwork of both our system and our culture. Nourish is rooted, deeply, in the care experience. We can only succeed in putting people first when we first start with their perspectives, experiences and outcomes of care.
In 2015 our CEO, Nuno Almeida, took part in a Tedx event in Bournemouth. The theme was ‘Creative Illumination’. It boasted a range of speakers and sectors, unified by their creative solutions for established challenges. Back then, the main focus for care technology was digitisation. While the conversation moved significantly forward since then, the roots of Nourish’s person-centred approach remain as relevant as ever. Digital care records are no longer an aspiration; they are a common feature. The goal of connected care plans is still pursued throughout each iteration of Nourish products as we continue to build towards a more informed, and informative, care ecosystem. You can even see the early ideas of data and AI application way back in 2015 when Nuno mentions ‘creating the right algorithms running on the data to help drive improved outcomes for people using care’.
Fundamentally, the talk ends with a focus on people. The people who utilise care services, their families, and the people who provide care. Nuno mentioned a few examples specifically as well as the ‘20 or so’ providers we were already working with. Because while ‘when’ we started can be debated, ‘how’ we started is clear. We started by working with care providers, and that is how we will always continue.
The past 10 years saw a lot of changes at Nourish Care. With expansions, integrations, and configurations galore.
The first three years were focussed on building out our functionality and scaling up to meet the needs of our rapidly increasing customer base. We went from 12 users at the start of 2015 to 428 in 2018! Thanks to user feedback we developed foundational features for the Nourish system during this time. Starting with interactive care plans in 2016, before focusing on data utilisation with Nourish Analytics launching in 2017 and Nourish Insights in 2018. Features and products we continue to develop and offer today!
By 2018 Nourish was operating in social care for several formative years. Over this time we learned about both the potential of our software systems, and the reality of social care technology.
So we co-founded CASPA with other care technology suppliers. The key goal of this group was the effective, safe and regulated proliferation of digital systems in social care. CASPA provided a resource for software suppliers to champion the benefits of our systems, like the exchange of information between care and health services, and other ways of digitally promoting continuity of care. This development reflected our ambition to positively impact social care on a larger scale through both our technology and our technological knowledge.
This undertaking almost immediately bore beneficial fruit. In 2020 COVID struck the world down, and social care providers across the UK stood up in response. CASPA demonstrated the power of care data utilisation to the UK government and the NHS. This data supported the forecasting and planning of future waves of the COVID virus to inform appropriate preparation and responses. A revelatory application of social care data. One that in turn helped drive improved care outcomes in many areas.
After the success of this initiative during COVID, CASPA pushed for further digitisation in social care. The establishment of the ‘Digitising Social Care’ programme was a direct result. Nourish was the first software supplier to qualify for the Digitising Social Care ‘Assured Solutions List’. The programme’s guide for approved systems available for purchase with local authority financial contribution.
The funding and expertise offered by this programme helped accelerate digitisation in social care throughout 2021. The following few years saw a myriad of digital platforms announce themselves to the sector. Each boasting its own benefits and unique solutions for long-standing social care challenges.
In response to this rapidly increasing selection of software we established the Nourish Partnership Programme (NPP) in 2022. We recognised that we can’t be the one source of every good idea in care technology. There are people working on brilliant technology all the time. Through the NPP we have, do and will continue to build connections with other care technology suppliers. Establishing a new aspect to our tradition of collaboration. Drawing on their specialisations and perspectives to support our software and offering guidance to Nourish users who are interested in expanding their technology ecosystem. Of course, we only integrate with those we align with, such as Altra, Found by Lottie, and e-Reception Book. This way we can ensure we are up to date with the best systems out there, as well as uncompromising on our commitment to keep people at the forefront of everything we do.
One of the biggest steps we took on this front was quite recent. Nourish Care acquired CarePlanner in 2023, nearly doubling our size and opening the world of home care to our technology. This acquisition was built on more than technological ambition. It brought together two care technology teams that already shared a design philosophy. A denominator of putting the person being supported first smoothed the combination of these teams. Following this acquisition Nourish became the most widely used care management supplier in the UK!
2024 was a year of growth across Nourish. We continue to add to our list of integrations and partners. We are building out all of our teams to reflect our ambition and responsibility. It took us a little time to fully acclimate to our increased size. Once these teams settled and people found the room to excel, we couldn’t help but look once more to the future.



The future is bright here at Nourish. Informed by tradition and unleashed by collaboration we have big plans and bold ambitions. Care technology is far more widespread than when we started. As a result we are moving from questions of digitisation to data utilisation.
When it comes to understanding data, and by extension AI, we are at the forefront in the care sector. We hired a team of well-educated and experienced developers, led by our Director of Data and AI, Sudha Regmi. We remain unwilling to rush to delivery with AI, as we continue to iterate and test AI models alongside Nourish users. This ensures we are not caught up in the hype of AI applications sweeping every industry in the world right now. But rather, we can walk assuredly, in step with care providers, to find the right applications of AI, and consequently, build the best apps for it.
This approach has stood us well over the past 10 years, and even recently has helped us develop new, exciting functionality for data management. Such as our Insight dashboards, and several exciting products coming soon.

These new products represented the next era for Nourish. Which in turn initiated an update to our naming conventions. Over the past 10 years we transitioned from working with care homes, to a wider range of care and support providers. As we expand our product range and the people we support even further, we realised we needed to update across the board while enshrining our guiding philosophy.
While we are expanding our range of products, our commitment remains the same. The people in receipt of care come first. Our new selection of products, the ‘Nourish Product Ecosystem’, reflect the changing world of care and support around us. They are targeted at specific challenges providers face. Offering effective digital solutions for a wide range of needs because we know no two people with support are the same. One size will very much not fit all. You need the right tools for the job, and the best people behind them to support you.
Each circle of the Ecosystem reflects a different focus for our products and the impact it will have on your community.
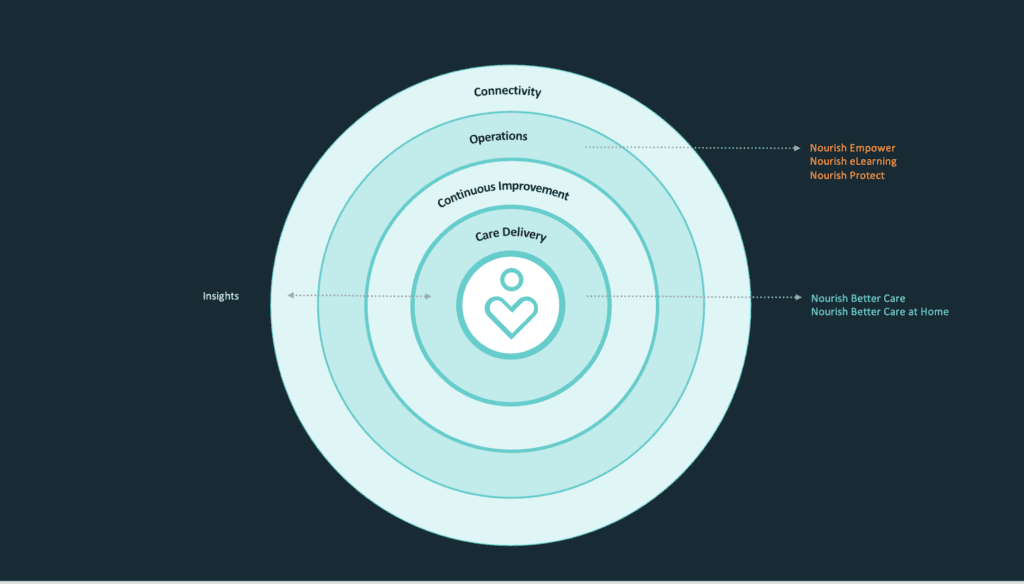
With each individual product developed and tested through co-production with our users to provide you with the innovations your community needs.
At the coalface of our new innovations is our product team. Under the stewardship of our Chief Product Officer, Matthew Stewart, we built a robust and creative product team. We understand care technology is at an inflection point in its development. We care presented with the opportunity to truly revolutionise how care is delivered and the outcomes it provides. Our team works alongside care providers, in Nourish tradition, to build this technology. Creating a cycle of iteration and feedback with a range of stakeholders from throughout the care process. Ensuring we have the perspective and experience of everyone who will be impacted by the care provided.
Who knows what the next 10 years holds?
At Nourish we are preparing the same we always have. By working with our users. Talking to people who live care every day. Bringing together technical expertise with human understanding and building solutions collaboratively across a range of relevant experiences. Reflection without action is simply indulgence. We look back with honesty so we can step forward with certainty. The past 10 years have not always been straightforward, but thanks to the people around us, we always know where we’re going.
Come join us for the next 10, it’s going to be one hell of a celebration.
Growth is a winding road. In October 2023 Nourish Care acquired CarePlanner Home Care Software. The merger brought together two leading social care software solutions for care homes and home care respectively. More than this, it brought together two teams who already shared a philosophy for collaborative software development, and a passion for supporting care providers on their digital journey. Over the past year we combined experiences, shared perspectives and continued to develop best in class functionality for our users, alongside our users, to drive better outcomes for everyone involved.
To celebrate an incredible 12 months, we caught up with some of the old guard from CarePlanner. We discussed the past year, what they’ve been up to, and why they’re excited for what’s still to come.



Combining two companies is a large, but delicate process. One that requires balancing different teams, responsibilities and skills with new opportunities and ambitions. CarePlanner’s Operations Director, now Nourish’s Director of Operational Excellence, Mark Gutteridge was instrumental throughout this transition.
“I oversaw the nuts and bolts side of bringing the two businesses together,” explained Mark. “Things like the processes, the way we work, the policies, making sure everything was aligned. That was the first six months. Since March of this year, my team are responsible for streamlining processes, putting in place new systems, and helping the business remain efficient as we continue to grow and onboard new customers.
“It was a big undertaking, and our guiding philosophy throughout was making sure we always asked the question ‘Why?’. It was a key case of prioritizing what was important and what would make a difference to our users. We brought the two companies together so we would both be stronger. We really wanted to deliver on that potential.
“There’s always a teething period with substantial changes like this. But once things settled down the benefits became obvious. We used to say to ourselves that CarePlanner wanted to do a lot of things, but they didn’t always happen as swiftly as we’d like. When you look at how swiftly we’re launching new features like our eLearning solution now it’s inspiring. We’re able to respond much more quickly and effectively to our users and their experiences. I think that it’s been crucial in terms of making sure we continue to support our users and provide a market-leading product and service. Which is a really exciting place to be.”
Understanding is central to building anything effectively. At Nourish and CarePlanner Home Care Software that understanding has always come from our users. Both companies boast team members with care experience. The combination of our Product teams, along with some experienced new leadership joining the fold, sharpened our focus, while at the same time unlocking whole new ideas to explore.
“The new structure builds upon our established user led approach with a wealth of experience and clinical expertise,” explained Product Manager Robert Baker. “Their focus on the clinical safety and the clinical side of the product is invaluable. It empowers us to understand the best practice around our software so we can shape our functionality to best respond to our user’s needs. We always want to stay as close to the lived experience of care as possible. Because it helps us tailor Nourish to the specific needs and use cases, some of which we’d never discover on our own!
“Fundamentally, the new structure keeps us focused on outcomes. Our attention is firmly on the problems we need to solve. Our teams have the resources and autonomy to respond to customer’s needs in a way that was previously unattainable. This means we can focus on developments for all sides of the Nourish platform, and any of the care types we support, with established care contacts and personal experience to guide us.”



Product teams focused on how to capitalise on our future opportunities to improve outcomes for our users. However, there remained the sizable task of bringing together the functionality the two companies already built for their respective platforms. We spoke to Lead Developer Martin Joiner about how they addressed this undertaking, and the benefits of bringing fresh eyes and open minds to old challenges.
“When we first joined together we were faced with two pieces of software with a lot of unique functionality,” explained Martin. CarePlanner’s home care software and Nourish’s residential. So, it was important to find the denominators. There are a lot of similarities between the systems as well. Features repeated across many platforms like: What does a profile look like? What information does it contain? How is an address formatted? General architecture like that. Lining these points up is a lot of work, but it is vital. We took small steps, one at a time to ensure we aligned the systems closely while still retaining the strengths of the previous structures.
“Of course, just like in care, the real strength came from our people. With so many new people to talk to and work with there are so many opportunities to share best practice. We can ask ‘Why?’ whenever our curiosity is peaked and learn from each other. There are few things better for a problem than fresh eyes and informed opinions. We all value understanding why we are building something. And this close relationship with the purpose of our development process is reflected throughout Nourish’s tech teams. Another key denominator that has shaped our success over the past year. Leading to new developments like TARS, Time Off and eLearning for Nourish home care users.”
Even on the technical level we find ourselves coming back to the importance of aligning on a human one. Personal connections define us all, especially when it comes to building productive, collaborative relationships in every aspect of our business. A maxim held true in both Nourish and CarePlanner.
CarePlanner Home Care Software may have been the industry standard for rostering technology. However, its reputation was built on more than technology, it was built on relationships. Nourish shares that focus on personal connections. A prerequisite requirement for the merger, and a substantial relief to the customer-facing teams on both sides of the acquisition.
“As Account Managers our first focus is always on the customers,” said Head of Account Managers Lauren Ware. “We build close connections with our customers because all Account Managers have dedicated accounts they work with. It delighted us to learn Nourish has the same approach. Thanks to the resources Nourish brings to bear on sector challenges our functionality and integrations have gone from strength to strength over the past year. This empowers Account Managers to unlock new opportunities for our users, and address long-standing challenges.
“It’s one thing to be told your philosophy aligns with another company, it’s a different thing to see it for yourself. Care is a fundamentally human undertaking. For all the changes the sector and we experienced over the past few years, that remains the constant. In Nourish we found partners who share that focus, and the results speak for themselves.”
The driving impetus of the acquisition was to make both solutions stronger. A combination of experience and insight to drive positive outcomes internally and externally for both businesses. One of the biggest changes this caused was for our support teams, whom we combined and specialised to best respond to our users in a timely and effective fashion.
“Bringing together the best of both Nourish and CarePlanner Support teams has been an exciting journey,” detailed Head of Technical Support Cian Connolly. “One that has strengthened our focus on what matters most, our customers. Over time, as the dust of the merger settled, we came to understand the needs of users and the strengths of our colleagues. This inspired us to develop two teams, Customer Support and Technical Support.
“With the move to dedicated Customer Support and Technical Support teams, we’re positioned to provide faster, more tailored solutions. Ensuring every interaction is both meaningful and effective. I’m incredibly proud of our team’s commitment and am excited for the future as we continue to raise the bar for customer experience in care technology!”
CarePlanner Home Care Software belongs to the past. But the people, platform and purpose that shaped it for over a decade remain in place. Committed to the same goals, and the same communities to whom we have always owed allegiance. Nourish is now the largest supplier of social care software solutions in the UK. With over 400k people supported through Nourish and 350k carers driving positive outcomes for their communities every day. A responsibility we all take great pride and purpose in.
The future remains an open horizon, and we have some fantastic company, and a stellar company, to join us on the journey.
The benefits of digital rostering go beyond efficiency. Optimisation is about more than driving shorter routes, it’s about driving positive outcomes as well. Staff scheduling is a complicated, and crucial part of delivering outstanding home care. It requires an in-depth understanding of your area, your community and your team. One that goes beyond simply managing spreadsheets. Truly great digital rostering software gives you the tools to bring all of your experience, data and empathy to bear on the challenge of staff scheduling in home care.
A good start is half the battle, though in home care it can often feel like an uphill battle at the beginning. Nourish Rostering’s overview puts you in the lifeguard’s seat; with a clear view of your service and the insight to notice trouble before it brews too long. Digital rostering centralises your vital information. You can schedule your clients’ needs and your carers availability as desired, ensuring that every appointment is covered, and every individual involved is well informed.
You can also fill your system with pertinent information about your service and the people who make it special. Clients can detail their needs, as well as their desires and ambitions. While your carers can include their skills, their interests and their passions. Separately these are useful silos of information, but together in one system they become influential drivers of positive care outcomes. These details can then be combined with geographic factors and clinical skills as you plan appointments and build runs to best match the needs and abilities of your care community.
That is the core power of digital rostering and home care software. The ability to bring together a wealth of information and put it at your fingertips. Unlock the expertise of your organisation by moving all the vital information from the heads and filing cabinets of your coordinators, onto a digital format. Ensuring no hour, need or opportunity gets overlooked when you are planning your care. This can feel like an uphill engagement indeed at the start! But once crested it brings speed, and specification, to your rostering process.
Of course, nothing in home care provision is ever straightforward. Which is precisely why home care software needs to be. Any care coordinator knows the unpredictability of a home care rota. Clients’ needs change over time, availability varies for all parties, and no one can ever be certain what awaits them just around the corner.
Any good home care rostering software needs to be reactive. Our drag-and-drop functionality is exactly that. It gives a succinct, yet detailed, overview of your schedule for the day, alongside the ability to quickly adjust appointments as necessary. Each client’s appointments are clearly shown, as well as the availability of your carers. This gives you the tools to quickly adjust when the inevitable changes need to happen. Digital rostering includes the ability to convey these changes as necessary with your team, so no one misses out on an update.
Crucially, you can make these decisions efficiently, with the weight of experience and the information of your system behind you. Our ‘Recommend’ a carer feature includes all relevant information on your calls so that you can send the right person to the right appointment every time. These factors include travel time and distance, specified to include mode of transport, familiarity with the client, experience and specific skills required and personal preferences of both the client and potential carers. Each data point further colours the picture of your care, and you can adjust the weighting of these points to match the unique needs of your community. Therefore you are not only planning efficiently, but effectively too, so you can continue to drive positive outcomes with your care.
Taking care of your team is a crucial part of optimising your staff scheduling. With digital rostering you can empower and inform your carers. Our all-in-one-pocket solution gives your carers a tool that has all the information they need to manage their day. An up-to-date schedule which shows not only where they need to be and when, but travel times in between. Allowing them to plan their routes effectively and adapt to changes with ease and efficiency.
Our new ‘Time Off’ feature helps you establish and manage your teams holiday accrual. Your carers can review and request time off through their app, promoting optimisation through centralisation of your processes. Decisions that once took half an hour can now be resolved instantaneously. This frees up your time to focus on people and outcomes, rather than balancing spreadsheets and calculators.
People are what drives care, and outcomes are how we measure our impact. Understanding that impact comes from understanding the way our care shapes lives. Staff scheduling plays a huge role in this, and call monitoring is key to ensuring your information is up to date and accurate when reviewing your home care rostering. Information like actual appointment times highlight the variety of key care indicators. Such as: consistent patterns in appointment length, travel times, travel mileage and more. You can record, review and report to best shape your appointments to the needs of your community.
This information can then be combined with other data points to optimise your digital rostering. Do you need to reduce the length of one appointment? Increase the length of another? Adjust runs to balance travel time? Or maybe change carers to account for public transport variances? When you digitise your processes, you position yourself to benefit from all the data you naturally accrue. With the right software, you can take full advantage of this opportunity to improve care quality, care efficiency, and care outcomes.
Digital rostering offers a range of benefits for your service. It lets you optimise the information you are already gathering and refine it to improve your outcomes as well as your efficiency. Time saving is a fantastic benefit on its own, and one that many care providers who are digitising their staff scheduling have experienced. However, there are far more benefits to unlock beyond efficiency. Benefits that involve everyone in your community collaborating effectively to change the lives of everyone in your community.
Thank you to Warrington Community Living for sharing the following article on their website. We love hearing how Nourish‘s digital platform is helping and improving care services across the country!
Embracing digital technology in the social care sector has many obvious benefits; not least time saving, more accurate note taking, simple reporting capabilities and a significant reduction in paper storage.
However, we are now also seeing that once care providers have fully integrated Nourish Care into their service, they are constantly finding innovative ways to utilise the technology.
Soon after the digital recording of care notes and updating care plans has become second nature, care teams become excited by the flexibility of the system and endless opportunities it encompasses.
The more time we spend with our care providers, the more we are impressed with the how forward thinking they are. Here are just a couple of examples of how our clients have been thinking outside the box when it comes to flexing the capability muscles of Nourish.
One home we recently revisited has started to record an interaction each day of wishing every resident a ‘good morning’. They also record their responses and any conversations that followed. It’s such a simple addition to their list of daily tasks, but encourages care staff to interact with the residents that little bit more, and on an emotional level. It also gives great insight into how the resident is feeling that day and can be a helpful indicator of their mental health.
Many of our clients provide care to pet owners, some of whom live in the home with them. Whether it’s cats, dogs, guinea pigs or chickens, carers have started to create daily records, and even care plans, for the animals. This is a fun and engaging way to use the system and ensures our fluffy and feathery companions are also fed on time, given any care they require and taken for those all-important walks.
Pets are often an integral part of a residents’ or service users’ life and happiness, and it’s just common sense to keep them healthy and happy too. Having care plans for the service’s pets also provides a great talking point when engaging with residents and their families, and we love how our care partners are using the system to encourage communication.
The flexibility of the Nourish system means that anything you want to personalise or remind staff of can be built into the daily records. Maybe Frank is trying a gluten-free diet; maybe Margaret likes a cup of tea while she reads in the afternoon; or perhaps Victor is going to start chair exercises once a week. Whatever the preference, goal or need, the daily records can reflect this, helping to keep the care team up-to-date of any changes.
Another innovative way we’ve seen care providers using the system is to also report maintenance issues. This could include task reminders, so that maintenance checks are completed, and even to ‘flag up’ maintenance concerns. For example, if a carer notices that a light bulb has blown, the carer can take a photo and note its location from a drop-down list of rooms on the Nourish system. They can then set a warning for the maintenance team who will see to the maintenance issue and turn off the warning when it has been resolved. It’s great to hear how the system is being used, not just to support care teams providing care, but also to support the smooth running of the overall service.
A final example of where our care partners have taken a unique approach to using our system is with regards to checking fire doors. We currently offer NFC tag technology, which many of our care and nursing homes use for night checks. These small tags are placed in the residents’ rooms so that when a carer completes a night check, they can tap their Nourish device onto the tag and it will record accurate information for when the check was completed.
Some of our care providers also use this technology to ensure fire doors are secure. The tag has been placed on the fire door, and when the relevant staff member taps their device onto the tag, a form appears which asks the staff member to check the fire door and record the task as complete or if action is required.
Our system was created to empower carers and support care teams to provide the best quality of care possible. However, we are so pleased that the flexibility of the system is encouraging care teams to think creatively and find new ways of making the most of the technology to support their care provision.
Last week, we attended yet another fantastic Dorset Care Conference, hosted by Care Management Matters at the Lighthouse in Poole. This time, we were invited to present on the role of digital in modern care delivery.
The fact that so many people joined us in the discussion was testament to the event organisers, but also showed that more and more care providers are considering how technology can help them improve the way they plan, record and report care.
Our care consultant, Luis Rela, shared some useful tips on how to approach the digital transformation process and how change management is key; while Juliana Jeffery from Luxury Care Group talked about her experience of using the Nourish system in her care home and how to overcome challenges.
The floor was obviously open for questions at the end, of which there were many. Here, we’ve shared a few of them.
Understandably, a banker in the audience wanted to know about the return on investment of going digital in care. Luis explained that there are both tangible and intangible benefits, and that care providers should think about the bigger picture when considering investing in a digital care management system:
“The tangible benefits are easier to define, of course. You only need to think about the paper you will no longer need to print, store, archive and shred to understand how those costs can be reduced over time.
“There are then intangible benefits such as time saved by recording notes digitally. Many of our care providers say they save at least one hour per carer each day because they don’t have to spend that time at the end of a shift writing notes and instead, record as they go. For some care organisations, this leads to a cut in the number of staff needed on each shift. However, what we find is that care providers instead maintain staff levels to increase the available one-on-one care for residents.
“In fact, one provider said that this decision led to them achieving an outstanding rating with CQC across three of the homes in the group.”
Juliana added: “There is also less time needed to get new or agency staff up to date with individual care plans and they have the time to get to know and spend time with that resident instead.”
So digital transformation is not primarily about driving costs down but improving the amount and quality of care that can be provided.
We were joined in the room by care providers of varying sizes, and many of them wanted to know how much time it takes to go from paper notes and care plans to digital ones.
Luis said: “Typically, it takes two months and we break down the transfer into stages; starting with daily notes and then care plans. However, this really depends on the size of the care home and whether it’s part of a group. If you take Luxury Care for example, they are still going through the process but that’s because they are doing one care home at a time. It also depends on whether we are developing unique features that work with their service. In one instance, a provider wanted to amend the digital care plan template to mirror that of the paper one, so we would do that first.”
Another member of the audience, who is already using Nourish in their care service, commented: “You could argue that there is never an end date once you are using an electronic care management system because you are always evolving and innovating. Every day we are learning something new and get more confident with the system, so every time we have a new idea, we integrate that into our process.”
Going digital obviously involves the use of physical handsets and electronic devices and some members of the audience were concerned that the responsibility of purchasing such equipment would be left to them.
As part of the Nourish service, we provide tablets for managers; handheld devices similar to Smart Phones for carers; and secure log-ins to our cloud-based system which can also be accessed from desktop. The number of devices needed will usually be the same amount of people you will have on each shift. The user will keep the device for the full duration of a shift, log out and handover to the carer taking over the next shift. Each member of the care team has their own log in with set permissions that have been pre-agreed and there are also log ins for agency workers.
Luis explained why this is the best way forward for everyone: “Care providers do not need the added pressure of having to find and purchase their own compatible devices and set them up. Because our software is completely adaptable to the care you provide, we get these ready for you prior to your training. We also have a dedicated technical support team on hand to help you with any queries.”
During her part of the presentation, Juliana explained how having a digital care management system in place had made communication between members of the care teams much easier and members of the audience wanted her to expand on that.
“Because it’s as easy as using Facebook and the device is with them all the time, it’s great for communicating important messages between members of the care team,” said Juliana. “Everyone can see and send messages through Nourish and handovers are now seamless. It’s been brilliant for ensuring everyone is informed immediately. For example, we also use this system to make sure we notify everyone of quality assurance audit results, which would otherwise have been left for meetings. Now everyone feels involved.”
Juliana also highlighted the added benefits of using these devices when recording notes: “We have carers who are not confident in writing notes or perhaps English isn’t their first language, so they love the speech dictation feature. As you speak, it records what you say.”
If you have any questions about the role of digital in modern care delivery and would like to find out how your care service can benefit, please give our team a call on 02380 002288.
If you work in care you will probably spend a great deal of time carefully planning and organising your care plans and pathways. So how do you know if your care plans are comprehensive enough to not only pass a regulatory inspection, but actively help those in your care receive effective support?
In order to help care providers avoid the many pitfalls that come with poor care plans, we’ve compiled a list of the top 12 mistakes poor care plans make and a subsequent list of methods you can use to avoid making them and ensure you always use effective care plans.
Each of the points we’ve made above has its own set of risks and requirements which all lead to a lower quality of care, but with the right approach, technology and techniques, care plans can be designed to avoid all of these pitfalls entirely.
Below we’ve detailed the best ways we’ve found to overcome these care plan pitfalls and how you can navigate through them yourself:
If you’d like to find out more about how Nourish can help you improve your care planning and avoid some of the pitfalls we’ve discussed above, then give us a call on 02380 002 288, get in touch with the team or book a demo.
Let’s face it, when you work in care there can seem to be an overwhelming number of different buzzwords, jargon and acronyms involved in the information you get given. This is especially true when you look at the practices involved with providing people with good quality care. Today we’re going to be looking into integrated person-centred care planning – we’ll help you to demystify the term and try to encourage you to adopt the practices it involves into your care provision.
To begin with we’ll be looking at what “person-centred” actually means in regards to care. Simply put, it’s a shortened way of expressing the creation of a series of activities aligned to specifically cater for a person and their requirements. In a way it’s how you choose to culminate your care pathways & activities in a bespoke manner to provide someone with actions, activities and results that are focused totally on the individual.
Person-centred, applies to care planning, when you take into account the clinical, holistic, desires, needs and wants of person when creating their care plans. It doesn’t stop there, however and in order to be truly person-centred, care plans must be created collaboratively with the person in control of the care interventions they want to accept, how they wish to receive them and designed to enable the person at every opportunity.
Here’s where things get a bit trickier. In order to provide integrated person-centred care planning, care professionals from all areas need to work together in order to ensure that the person in care has a seamless provision of their care, no matter the setting. When you have a person whose care requires the interventions from a variety of different social care and healthcare organisations, this can become fairly complex and has only realistically been achievable with the introduction of electronic health records and electronic care planning systems.
Here at Nourish we focus firmly on empowering person-centred care for those who provide and are in care. You can read more about our vision in our recent article on “framing personhood to manage frailty, needs and wants” from our founder Nuno Almeida. It’s why we’ve designed the Nourish system from the ground up to help enable people to receive tailored care and empower carers to do just that.
Nourish’s care planning system helps care workers, care teams, care managers and senior care providers with person-centred care planning by:
Our team of experts are always happy to help talk through how the Nourish system empowers care teams and care providers – talk to us today to find out more.
At Nourish there are a number of principles that guide our work. Firstly we understand the importance of planning in care, which is why we put care plans at the heart of what we do. Establishing a care plan is key to providing truly personalised care, so we designed Nourish to make that process as smooth as possible.
No two care settings are ever the same, which is why Nourish is flexible and customisable. Our approach is to tailor Nourish to work for care teams, not the other way round. So if a care team has well-established care plans that they are already using, we work with the team to take those care plans online with Nourish – creating the same order that carers are used to. Other settings may prefer to use Nourish care plan templates and then customise them to the care they provide – from nursing care to dementia care to domiciliary care to learning disabilities.
Secondly we use clear, user-friendly design to allow Nourish to fit into carers’ daily work. Care plans can be set up to generate tasks on a daily schedule – for example, if part of a person’s care plan is to monitor a person’s weight loss, daily tasks can be set on the timeline to check nutrition and food intake. Carers have told us time and again that the two hours they used to spend at the end of a shift on paperwork has simply gone, because by the time the shift has finished they have already made all the notes they need to.
Thirdly, care is provided not by a single person, but by a circle of care. Within a residential setting, this may involve the care team, visiting medical staff and family. In home care settings, friends and neighbours may also play a role. With Nourish, notes can easily be made by each person providing care. That information is then stored and organised in the care plan logs in a clear way so that others can access it when they need to.
With all this in place, generating reports no longer involves spending hours retrieving files from the shelves but can be done with just a few clicks, before, after or even during a CQC inspection if required. Care plans can easily be reviewed and audited, which is also vital when it comes to inspection. Reviews may be scheduled, but care teams also have the flexibility to react to changes in a person’s condition which may trigger the need for a care plan review.
Care requires both consistency and flexibility. We designed Nourish to support those needs. Which means care teams can get on with doing what they do best – provide the real, human, compassionate care that enables the people they care for to enjoy the best quality of life possible.