Our Chief Marketing Officer Lee Gilbert recently joined David Thompson and Natasha Bone of Rehability Care for a two part episode of their podcast, Social Care Chronicles.
‘Digital Care Planning in Action: Transforming Lives with Nourish’ explores how we are working with our users to reshape the future of social care.
Part 1 of the episode covers a range of topics from reducing paperwork to empowering individuals with learning disabilities, autism, and mental health conditions. Our conversation uncovers the real-world impact of person-centred, data-driven care.
You’ll learn
Whether you’re a care provider, tech innovator, or policymaker. This episode is packed with insights on digital transformation in social care.
Don’t miss Part 2, where we dive deeper into implementation, integration, and what’s next for the future of digital care!
Part 2 premieres at 11:00 A.M. 10th September 2025.
In Part 2 we explore
Learn more about the innovations at Nourish. And how we’re building for the future of social care on our Articles page.



Birthdays are a natural cause for reflection. As Nourish Care celebrate our 10th we find ourselves looking to both the future and the past to better understand where we are today. For 10 years, ever since we got our first customer, Nourish has been proudly supporting care providers across the UK and beyond.
Growing alongside our users, increasing the functionality of our platform and expanding the range of care types we work with. Throughout this journey we remain connected by a singular focus, a golden thread that runs through every iteration and evolution of Nourish. The idea that the people who receive care come first. This commitment to care and foundation in coproduction defines our past and decides our future. As we look forward to a litany of possibilities, from data and AI, to family connections and institutional integrations, it is our focus on people that matters most. As is tradition.



Okay, technically, we are actually closer to 14 than we are to 10. The seed for Nourish was first planted in 2011. This seed of an idea would spend four years flowering into the first iteration of Nourish that was officially launched with our first customers in 2015. These four years laid the groundwork of both our system and our culture. Nourish is rooted, deeply, in the care experience. We can only succeed in putting people first when we first start with their perspectives, experiences and outcomes of care.
In 2015 our CEO, Nuno Almeida, took part in a Tedx event in Bournemouth. The theme was ‘Creative Illumination’. It boasted a range of speakers and sectors, unified by their creative solutions for established challenges. Back then, the main focus for care technology was digitisation. While the conversation moved significantly forward since then, the roots of Nourish’s person-centred approach remain as relevant as ever. Digital care records are no longer an aspiration; they are a common feature. The goal of connected care plans is still pursued throughout each iteration of Nourish products as we continue to build towards a more informed, and informative, care ecosystem. You can even see the early ideas of data and AI application way back in 2015 when Nuno mentions ‘creating the right algorithms running on the data to help drive improved outcomes for people using care’.
Fundamentally, the talk ends with a focus on people. The people who utilise care services, their families, and the people who provide care. Nuno mentioned a few examples specifically as well as the ‘20 or so’ providers we were already working with. Because while ‘when’ we started can be debated, ‘how’ we started is clear. We started by working with care providers, and that is how we will always continue.
The past 10 years saw a lot of changes at Nourish Care. With expansions, integrations, and configurations galore.
The first three years were focussed on building out our functionality and scaling up to meet the needs of our rapidly increasing customer base. We went from 12 users at the start of 2015 to 428 in 2018! Thanks to user feedback we developed foundational features for the Nourish system during this time. Starting with interactive care plans in 2016, before focusing on data utilisation with Nourish Analytics launching in 2017 and Nourish Insights in 2018. Features and products we continue to develop and offer today!
By 2018 Nourish was operating in social care for several formative years. Over this time we learned about both the potential of our software systems, and the reality of social care technology.
So we co-founded CASPA with other care technology suppliers. The key goal of this group was the effective, safe and regulated proliferation of digital systems in social care. CASPA provided a resource for software suppliers to champion the benefits of our systems, like the exchange of information between care and health services, and other ways of digitally promoting continuity of care. This development reflected our ambition to positively impact social care on a larger scale through both our technology and our technological knowledge.
This undertaking almost immediately bore beneficial fruit. In 2020 COVID struck the world down, and social care providers across the UK stood up in response. CASPA demonstrated the power of care data utilisation to the UK government and the NHS. This data supported the forecasting and planning of future waves of the COVID virus to inform appropriate preparation and responses. A revelatory application of social care data. One that in turn helped drive improved care outcomes in many areas.
After the success of this initiative during COVID, CASPA pushed for further digitisation in social care. The establishment of the ‘Digitising Social Care’ programme was a direct result. Nourish was the first software supplier to qualify for the Digitising Social Care ‘Assured Solutions List’. The programme’s guide for approved systems available for purchase with local authority financial contribution.
The funding and expertise offered by this programme helped accelerate digitisation in social care throughout 2021. The following few years saw a myriad of digital platforms announce themselves to the sector. Each boasting its own benefits and unique solutions for long-standing social care challenges.
In response to this rapidly increasing selection of software we established the Nourish Partnership Programme (NPP) in 2022. We recognised that we can’t be the one source of every good idea in care technology. There are people working on brilliant technology all the time. Through the NPP we have, do and will continue to build connections with other care technology suppliers. Establishing a new aspect to our tradition of collaboration. Drawing on their specialisations and perspectives to support our software and offering guidance to Nourish users who are interested in expanding their technology ecosystem. Of course, we only integrate with those we align with, such as Altra, Found by Lottie, and e-Reception Book. This way we can ensure we are up to date with the best systems out there, as well as uncompromising on our commitment to keep people at the forefront of everything we do.
One of the biggest steps we took on this front was quite recent. Nourish Care acquired CarePlanner in 2023, nearly doubling our size and opening the world of home care to our technology. This acquisition was built on more than technological ambition. It brought together two care technology teams that already shared a design philosophy. A denominator of putting the person being supported first smoothed the combination of these teams. Following this acquisition Nourish became the most widely used care management supplier in the UK!
2024 was a year of growth across Nourish. We continue to add to our list of integrations and partners. We are building out all of our teams to reflect our ambition and responsibility. It took us a little time to fully acclimate to our increased size. Once these teams settled and people found the room to excel, we couldn’t help but look once more to the future.



The future is bright here at Nourish. Informed by tradition and unleashed by collaboration we have big plans and bold ambitions. Care technology is far more widespread than when we started. As a result we are moving from questions of digitisation to data utilisation.
When it comes to understanding data, and by extension AI, we are at the forefront in the care sector. We hired a team of well-educated and experienced developers, led by our Director of Data and AI, Sudha Regmi. We remain unwilling to rush to delivery with AI, as we continue to iterate and test AI models alongside Nourish users. This ensures we are not caught up in the hype of AI applications sweeping every industry in the world right now. But rather, we can walk assuredly, in step with care providers, to find the right applications of AI, and consequently, build the best apps for it.
This approach has stood us well over the past 10 years, and even recently has helped us develop new, exciting functionality for data management. Such as our Insight dashboards, and several exciting products coming soon.

These new products represented the next era for Nourish. Which in turn initiated an update to our naming conventions. Over the past 10 years we transitioned from working with care homes, to a wider range of care and support providers. As we expand our product range and the people we support even further, we realised we needed to update across the board while enshrining our guiding philosophy.
While we are expanding our range of products, our commitment remains the same. The people in receipt of care come first. Our new selection of products, the ‘Nourish Product Ecosystem’, reflect the changing world of care and support around us. They are targeted at specific challenges providers face. Offering effective digital solutions for a wide range of needs because we know no two people with support are the same. One size will very much not fit all. You need the right tools for the job, and the best people behind them to support you.
Each circle of the Ecosystem reflects a different focus for our products and the impact it will have on your community.

With each individual product developed and tested through co-production with our users to provide you with the innovations your community needs.
At the coalface of our new innovations is our product team. Under the stewardship of our Chief Product Officer, Matthew Stewart, we built a robust and creative product team. We understand care technology is at an inflection point in its development. We care presented with the opportunity to truly revolutionise how care is delivered and the outcomes it provides. Our team works alongside care providers, in Nourish tradition, to build this technology. Creating a cycle of iteration and feedback with a range of stakeholders from throughout the care process. Ensuring we have the perspective and experience of everyone who will be impacted by the care provided.
Who knows what the next 10 years holds?
At Nourish we are preparing the same we always have. By working with our users. Talking to people who live care every day. Bringing together technical expertise with human understanding and building solutions collaboratively across a range of relevant experiences. Reflection without action is simply indulgence. We look back with honesty so we can step forward with certainty. The past 10 years have not always been straightforward, but thanks to the people around us, we always know where we’re going.
Come join us for the next 10, it’s going to be one hell of a celebration.
Change, from social care to sofa cushions, is a constant.
For a decade we at Nourish Care have been proud to help shape that change in social care. When we launched Nourish care technology was in its infancy. A vague selection of ideas and applications attempting to address a complex collection of people, processes and promises. Our approach was rooted in our understanding, bringing together our technical expertise with our personal experiences of care to ensure that care technology always put people first. From the very beginning, Nourish has been built on one simple but powerful belief: the person supported matters most.
This belief is why we develop all our functionality through coproduction. Our commitment to collaboration is felt throughout our system. Thanks to this approach our understanding of care is deeper, our experiences wider and our expertise sharper than when we started. We continue to grow with our users just as social care technology enters its awkward adolescence. The past decade has shown us the potential for technology in social care, while Nourish users have revealed to us the best applications for our software, opening our eyes to the opportunities for supporting positive change in the wider system of care. In response, we are releasing several new Nourish products to support the wider care sector.
This expansion of our application is rooted in keeping people at the centre of our systems. We know growth demands structure, scaling demands clarity, and crucially, care demands trust. Structure can be built, clarity provided but trust, trust must be earned.
Nourish Care is the longstanding name of our platform and our business. More than that it is a promise, a commitment to community, coproduction and care. We will be changing the name of our platform to accommodate the new products we have developed for the wider system of care.
We are keeping the promise.
Our new naming convention reflects our renewed focus on people. Technology should feel as natural as the care it supports. That’s why we’ve ensured that every product name reflects not just what the platform does, but how it makes people feel.
Nourish Care has become Nourish Better Care
It’s important to remember where you started! Nourish Better Care is the most trusted and customisable care management system for residential providers in the UK.
Nourish Rostering has become Nourish Empower
All the tools a home care provider needs to support their community and manage their service.
Nourish Community has become Nourish Better Care at Home
Combining the mobility and admin of Nourish Empower with the industry leading point of care functionality of Nourish Better Care to support effective processes and drive improved outcomes.
Nourish Mobile Device Management (MDM) has become Nourish Protect
Keep your devices secure and your community’s data safe with our mobile device management system.
Nourish Insights
Get the full picture of your service with our data dashboards so you can make more informed, more effective decisions.
Nourish eLearning
Available through our home care platforms, Nourish eLearning offers an integrated, accredited by CPD and Skills for Care, library of care courses for your team to utilise, supported with real time reporting.
Transform your approach to incident management with tools that enable you to capture, report on, and learn from incidents.
Nourish Transparency enables services to align needs, staffing, and funding from the very start and keep them aligned as things change.
Nourish Care will continue to be the name of our business, with the specific names of products reflecting the impact they deliver for care providers and your communities.
We are not the only ones changing. You are too. Our users have changed so much over the past decade, through digitisation, updated regulations, and new legislation, without ever losing sight of the people that make care so special. With our new, multiple product approach, we are establishing our foundation for future growth alongside you. So, we can best respond to the needs of today, and the challenges of tomorrow.
No two people with support are the same. Uniqueness is the blessing, and the curse of social care. One size will very much not fit all. You need the right tools for the job, and the best people behind them to support you.
To make it easier to find the right products for your community we created the Nourish Product Ecosystem. Each circle reflects a different focus for our products and the impact it will have on your community.
Care Delivery – For Feeling Supported
Technology that steps back, so care can step forward.
Continuous Improvement – For Feeling Assured
Because confident carers create safer, more consistent outcomes.
Operations – For Feeling Secure
Supporting care teams to be prepared, skilled, and sure of what comes next.
Connectivity – For Feeling Connected
Bringing together every piece of the care puzzle around the person.
This approach goes beyond categorisation. It lays the foundation from which every new product, every innovation, and every solution we launch builds towards something bigger.
Most importantly, it ensures that as we scale, we never lose sight of what made us great, keeping the person supported at the centre of care.
Imagine a healthcare system where care teams feel empowered instead of overwhelmed. Where families feel reassured instead of disconnected. Where people receiving care feel safe, valued, and heard.
That’s the world we’re building.
And we’re not waiting.
We have coordinated internally
So our teams live and breathe this philosophy.
We are communicating externally
So our customers feel the impact as soon as possible.
We will continue to co-produce
Because technology should evolve with the people it serves.
Change is a constant, a promise, and a challenge. One that can only be met in the same way we always have here at Nourish, by working together. Coproducing our products so that people are always at the centre of everything we design, develop and do. Because after all, change, like care, is human.
We’ve got lots of exciting plans coming soon, if you want to build the future of social care with Nourish, contact us directly today.
When Wes Streeting announced his three key shifts for the National Health Service (NHS) at the Labour Party Conference at the end of September social care’s ears were burning. A move from analogue to digital, hospital to community and sickness to prevention is a move towards care. Clearly social care has a big part to play in the future of the NHS. And technology plays a crucial role in the future of social care. When applied correctly digital solutions empower us to improve both efficiency and outcomes. Which offers care technology a central role in the government’s ongoing attempts to stage a digital revolution in health and care. We all know the why, given social care’s enduring challenges. It is uncovering the precise, who, what, when, and how of the matter that remains something of a mystery.
We recently headline sponsored the Home Care Association (HCA)’s Tech & Homecare conference. A day of insights, inquisition and understanding for leading home care providers and technology suppliers. On the day our CMO, Lee Gilbert, hosted a panel featuring a who’s who of digital rostering and AI suppliers discussing data, while The King’s Fund’s Pritesh Mistry joined HCA’s CEO Dr Jane Townson OBE to ask, ‘How can technology solutions help move care closer to home?’. The latter a conversation underpinned by the recently published, Nourish Care sponsored, study exploring ‘The reality of, and potential for, digitally enabled care in the community’. Reflecting the collaborative spirit of co-development that defines modern, outstanding care, these conversations detailed a variety of ongoing efforts to move social care from analogue to digital. Their success, their missteps, and the road still ahead.
Chair: Lee Gilbert, CMO, Nourish
Nuno Almeida, CEO, Nourish
Steve Sawyer, Managing Director, Access Group
Robin Batchelor, CEO, everyLife Technologies
Matthew Bond, CEO, Borderless
Abeed Mohammed, Co-founder, Birdie

There is already a wealth of positive examples of technology improving care quality. Providers applied digital solutions to a selection of the challenges they face. Both The King’s Fund research, and each of the panellists, presented their own positive instances. Pritesh detailed several different, key, areas that are already befitting from digital solutions, such as communication, care co-ordination and personalisation. Dr Townson added to this during their conversation, highlighting some Local Authority’s recent adoption of ‘magic notes’ as an example of technology changing people’s lives.
The panel built upon these cases with a specific focus on utilising existing data in systems. Matt Bond shared how Borderless share and aggregate data to pass benefits to individual people by finding the gaps in your existing service. The other four panellists all pointed to the efficiency their respective rostering platforms bring to care providers. When Robin Batchelor brought attention to the current inflection point in care technology it resonated around the room. Nuno Almeida agreed, “We’ve spent 14 years building the foundations. It’s not rocket science; the rocket science lies in your ability to react to needs.”
That is the crux of the matter, when we move from analogue to digital, we have to retain our focus on people’s needs. The ability to react to these needs is defined by our ability to engage with them. One of the biggest fears about moving from analogue to digital is based in the apprehension of losing the human touch that has always guided health and care in the UK. A fact reflected in two of the recommendations from the King’s Fund’s research. The need to ‘Shift culture to embrace the public’s digital capability’ and ‘Support staff to embed tech in their roles’. Neither of which are groundbreaking discoveries, but do require fresh ideas to address. Such as Scottish Care’s Care Technologist role. We know the potential of carers, their adaptability and commitment to any idea that can improve outcomes for their community.



What we need to do is make engaging with, and championing, care technology a simpler process. Which is not something that can be done overnight. “Asking people what is important to them is the biggest gap in our data,” admitted Nuno during the panel. “But this is also a big opportunity for us, asking, ‘What will really make a difference?’” The more we can involve people in the design process, the more ‘frontline’ feedback we can apply to our development. This co-production keeps people at the heart of care technology, which is crucial as we move to put technology at the heart of care.



Dr Townson concisely summarised this issue during her talk with Pritesh. ‘Technology for technology’s sake is not progress’. Innovation cannot be disruption in care, the standard approach for technology entering a new sector. The responsibilities are too great. We have to understand the barriers and develop enablers for adoption in the workforce and communities they support. Any one software solution aiming to promote wrap around care and support needs to ask itself a simple question. ‘How will the care providers work alongside our tech?’
Pritesh highlighted the need for this focus in his research with The King’s Fund. One of the recommendations from this research underlines the need to ‘develop strategies for co-developing digitally enabled services’. Specifically raising the point that developing a strategy for co-development and patient-led service design will help to direct digital service development and strategy. While this suggestion calls for action from ICSs, ICPs, the NHS and the Department of Health and Social Care (DHSC), it speaks to all digital suppliers and providers in social care. The move from analogue to digital in care must involve people at every step, or it is sure to get lost.
Nuno spoke about the need to ‘crawl, walk, then run, to get to data quality’. A process that rings true for all forms of digital technology. When The King’s Fund recommends ‘A national vision to guide local decisions’ it is not calling for a direct mandate. It is asking for a personalisable framework. ‘A guiding national vision, with local flexibility as to how it is achieved. One that will help to align the efforts of technology innovators, health and care providers, and leaders designing improved community-based services.’
The HCA’s conference was an example of just that endeavour. A selection of leaders, creators and providers sharing experiences and ambitions to help shape the future of care as we move from analogue to digital. One based in the commitment to collaboration that makes care the beating heart of our communities. After all, if you’re going to solve a mystery machine, it’s best to do it with a gang.
‘Co-production’ is a long-standing practice and a newly minted hot topic in social care. It is based on our ability to involve all relevant people, or ‘stakeholders’ as they say in corporate meeting rooms, in the process of care design. It guarantees that the people who are utilising a care service are involved in the production of that care. An undertaking that lies at the heart of person-led care.
If people with support, families and commissioners expect this of care providers, then it is only natural that those care providers should demand it from their software suppliers as well.
At Nourish Care, co-production is central to our design process. It bridges our technical expertise with our user’s care experience to produce effective, efficient solutions. Our user’s input guides our development, with feature requests, feedback forms and beta testing being just some of the essential ways we keep our user’s experience central to our development.



The latest Innovation to emerge from this process is our new ‘Time Off Management’ functionality for Nourish Rostering and Community. We know that managing rosters is one of the most demanding aspects of providing home care, for both coordinators and carers. We developed our Time Off Management feature to address these challenges directly based on extensive user feedback, advice and industry insights.
Our new functionality is designed to simplify your time off processes, making it easier to manage leave, maintain coverage, and ensure a smooth operation for everyone involved.
The features of our new Time Off functionality are all directly tied to the feedback and input of our users.
Holiday schemes allow for a group of settings to be built and then applied to relevant carers. This grants customisability and flexibility to coordinators while removing the need to configure each carers holiday settings individually. You can group holiday accrual, reference periods, pay methods and more to make the complexities of specificity a simple activity.
We found the denominator of our feature requests for time off functionality was customisability. It is the most effective way to support the varied and at times unpredictable home care provider’s scheduling needs.
Features like year start dates for holiday accrual, carry over time settings for different time off types and pay calculations all vary from service to service, and across different governments and geographies. For example, the holiday pay reference period in the UK is 52 worked weeks while in the Republic of Ireland it is a 13-week reference period. It was vital we build these features with the freedom for our users to customise the settings and wrap them around their unique service.
We have also included a manual entitlement adjustment for coordinators for precise control when desired. A need we discovered when talking to a lot of the participants in our beta testing phase.
Of course, it wouldn’t be Nourish without analytics and reporting functionality as well. We have a fantastic analysis page to help administrators keep track of their carers time off. It includes a calendar view of all booked, requested and refused time off, a chart of absence types e.g. holiday, sick, bereavement, a table view of the adjustments made to their carer’s entitlement, a table view of requests, their status and the option to filter or edit them as desired.

We built several key new time off functions into our carer app as well. This gives more insight and control to carers. With our new Time Off Management functionality carers can request leave directly from the rostering app, simplifying the process of requesting time off for a variety of reasons including holidays, sickness and bereavement.
Carers can use the app to review their remaining time off allowance and keep track of requests. We centralised all this information to further our app as the leading carer support platform in home care. Information is power for a carer on the go and with this new functionality we continue to develop our ‘all-in-one pocket’ solution. It provides an overview of their currently accrued time off and helps to make the process of defining availability and accrual more straightforward for everyone involved.
Carers can use the app to review their remaining time off allowance and keep track of requests. We centralised all this information to further our app as the leading carer support platform in home care. Information is power for a carer on the go and with this new functionality we continue to develop our ‘all-in-one pocket’ solution. It provides an overview of their currently accrued time off and helps to make the process of defining availability and accrual more straightforward for everyone involved.
For non Nourish users who want to learn more about our approach to co-production and working with us to support their home care service, book a demo.
We have spent years working on our rostering system to make this as quick and straightforward as possible. Something we could only achieve thanks to co-production with our users through our beta testing processes. We spoke to Samantha Rabvu, Care Manager for TLB 24/7 Healthcare, about her experience participating in our Time Off Management beta.




“We were paper based for annual leave requests,” explained Samantha. “Which meant someone had to fill in a form and scan it or take a picture of it. Then we were constantly just printing so I could give it to the person who’s approving annual leave. So when the offer to take part in a beta test for time off came along I just thought. ‘I don’t know what it is going to look like, but it sounds like something we could really use.’
“It offered the chance to cut out the middle man, the printing, and give power to both our carers and our coordinators. It was the chance to move to real time updates, rather than requests from a variety of platforms. In December last year we had a whole lot of annual leave requests. Honestly, we lost track of them due to the volume and variety of requests. Which was a major concern for us. So, when I saw that you were building something that could show us how many people are asking for time off and those who are already taking time off before approving any more, it was a game changer for me.”
“I felt very involved,” said Samantha. “I could see the team was really drawing out our feedback with the questions they asked. ‘How is it going?’ ‘How are you guys using it?’ ‘Are there any adjustments we should make?’ I felt like a real partner that the things were saying were being considered. When we saw one of our suggestions in the next update it was amazing. I’m sure I wasn’t the only one suggesting it, but it was awesome.
“We were involved throughout the process, even my team here was quite involved. Any issue that they had, they knew they could bring it to me, and I would pass it on. That way we always got things resolved.”
“They were on it,” said Samantha, “They were on the money. It was so easy. If there was an issue, I’d send a screenshot and they were on it, we looked at it in depth, it was awesome. I had a main contact point but worked with several different members of your team. I just knew that they were there. They had our back, no matter what.
“They are awesome, friendly, approachable, and we could rely on them 100%. Even the way bad news came was awesome. When something wasn’t ready, we always knew that it was still in development, it’s just not ready yet. We understood because of the communication, and we trusted your team.”
“We’re on the right track,” said Samantha. “This was a great starting point for me. It was fantastic. Even though I was a little unsure at the start, digital wise, this isn’t something i had a lot of experience with. The process helped us to develop skills and tactics on how to navigate the rest of the digitalization roadmap, which is great.
“So, I’m hopeful. I’m looking forward to it, it’s exciting, because I feel involved in the process. I feel like we are growing with you, and we can build something great together.”
The future of social care will be shaped by co-production throughout the entirely of our sector. Lived experience, collaboration, data sharing, all fold together under the guiding philosophy of teamwork and community. We received over 150 feature requests for more advanced time off functionality. Which was the starting point of our development cycle, and a continuing example of our approach to digital social care solutions.
We still have a long way to go, and we are very excited about the journey. Why don’t you join us?
Home care software is baked into the future of social care. We witnessed a huge increase in the uptake of digital systems across social care over the past 3 years. A change accelerated by government policy and funding. This considerable uptake brought with it a range of advantages and benefits for care providers. For example, digital rostering systems like Nourish help providers to simplify processes, reduce administration times and record more detailed information. With digital systems becoming commonplace in social care there has never been a more urgent time to switch to Nourish. Admissions for the funding available through Integrated Care Systems will close at the end of November. Even for those providers who are still getting up and running choosing the right digital rostering system is crucial for many reasons.
Nourish gives you the tools to take full control over your home care administration. This means more than rosters designed for simple and swift use. It means a robust system compiling the wealth of data your teams naturally gather to provide you with a clear overview of what is happening in your community.
With Nourish you can schedule your carers and clients up to four weeks in advance. Repeating these schedules with ease to improve consistency across your service. Of course, as all home care administrators understand, nothing ever goes totally to schedule. Nourish home care rostering is designed with drag and drop functionality that makes changing your schedule on short notice easier than ever. Our home care software includes a ‘recommend a carer’ feature that is scored based on a range of data points you choose and weight. Such as: familiarity with client, travel to appointment and relevant skills for the appointment’s tasks. So, you can adjust quickly, decisively and with confidence.
Digital rostering offers benefits beyond simplifying existing paper processes. Nourish Rostering and Community unlock a range of features that put new innovations and fresh information at your fingertips. Call monitoring is a straightforward way to record actual appointment times. Nourish includes geographic location and a range of electronic call monitoring options to suit your needs. Care providers, especially those with local authority and council contracts can attest to the benefits of a robust call monitoring system.
Crucially, with a quality home care software like Nourish, you can access data at a level previously unattainable with paper. This data is easily presentable and evidencable in trends and reports. You can track different factors regarding your team and community to give you a more detailed overview of your service. These details, like travel times and medical administration, can be fed back into your service to drive positive outcomes. As well as acting as informative evidence for your regulator.
Nourish home care software supports care providers across your service. Home care requires a great deal of administration and organising. Beyond the design of schedules and care packages there is the crucial matter of making sure everything is in order, and everyone is properly paid. This can be quite daunting for people when they are just setting out their new home care service. Especially those less familiar with operating a business.
Our invoicing and timesheets are a simple way for you to organise your payroll. You can use Nourish to set specific pay rates and charge rates, to match with the responsibilities of your teams and the services they provide. Our home care software includes comprehensive time-off functionality. Allowing you to set the rate at which holiday is earned, and for your team to manage and request leave through the Nourish home care app.
Big changes are rarely simple. But with the future of social care coming at us at its current speed, now is the simplest time to do it. The best home care software comes backed up with a human team. People who will work with you to make sure you get everything you need from your system. At Nourish we pride ourselves on being person-led and community-centred. We are incredibly excited about the future of social care, and we’d love to share it with you.
If you want to find out more about working with Nourish book a demo!
Professional development in social care is a fundamental building block for the future of our sector. Skills for Care’s ‘Workforce Strategy for Adult Social Care’ details several benefits of investing in care eLearning and training. These range from driving quality care to improving your ability to recruit and retain care workers. Fundamentally, the impact of professional development in social care reverberates through every aspect of your service. At Nourish Care we appreciate that there are many white papers, plans and strategies for improving social care. The challenge lies in finding the time, energy and platform to pursue them.
That’s why we are so excited to announce the latest member of our Nourish Partnership Programme, MyAko. MyAko are a Skills for Care and CPD accredited eLearning provider. We’ve partnered with them to deliver an all-in-one digital learning solution for home care agencies. Our platform links directly to the Nourish Rostering app. Enabling easy access for your staff and offering a streamlined way to manage training compliance. With over 100 thousand active users MyAko’s comprehensive library of courses covers a range of topics. Their platform has over 60 courses dedicated to professional development in social care, including Care Certificate, Safeguarding Adults and Children, and Moving and Handling People. Crucially, they are committed to continually developing and adding to the courses they provide.



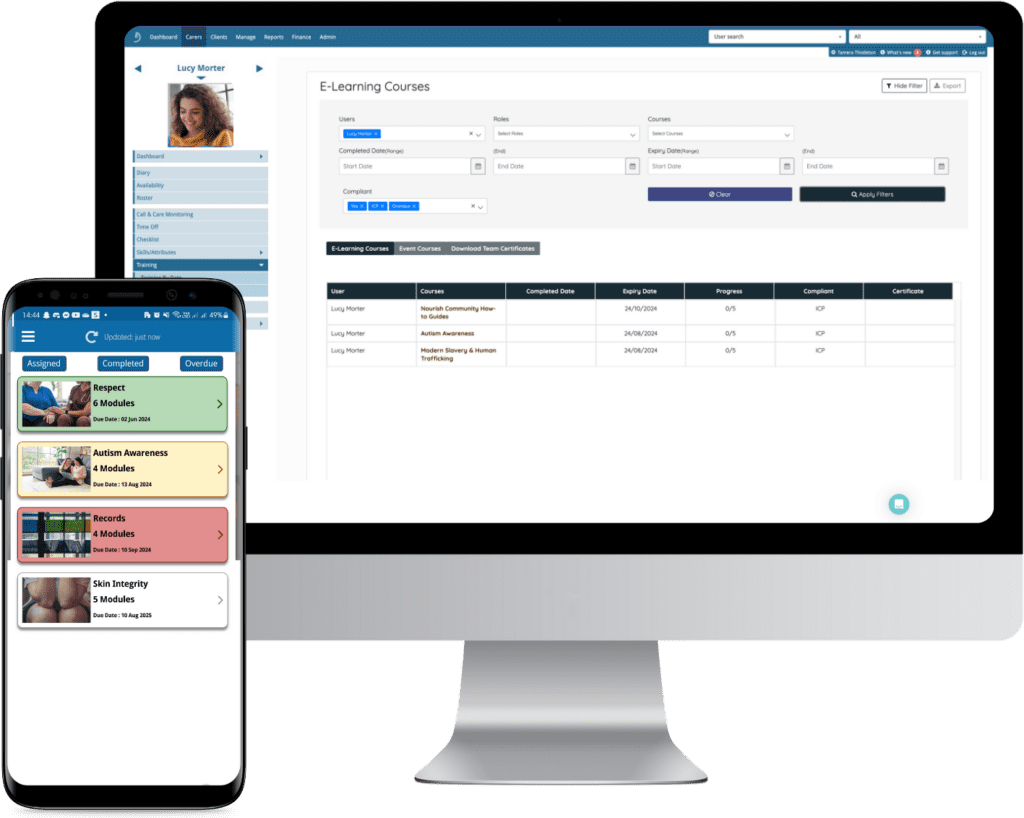
We linked our home care rostering platform directly with MyAko to streamline your experience. This means you will have full access to a range of MyAko’s care eLearning features directly through Nourish. Shape the development of your teams by assigning and tracking courses. You can keep an eye on progress and monitor compliance throughout the duration of these courses for more organisational oversight as well as downloading certificates upon course completion. This gives you a throughline for recording, reviewing and reporting your teams training. So not only can you provide professional development in social care, you can evidence it as well.
Signing up is as straightforward. Simply head over to the Admin eLearning section and click the “Sign Up” button to get started. Once activated you can set up Course Assignment Rules to establish mandatory courses for your team, based on your existing regions or job titles. It is also possible to set up unique training per person when it’s needed. You’ll find this option in the Individual Course Assignment section.
You pay for courses with course credits, which can be bought directly through the platform. The cost of courses ranges from 1-3 credits depending on the topic. This gives you the flexibility to pick and pay for courses suited to your company’s needs. There is a report available for your course credit purchases as well to help you keep track of your costs. You can also establish pay settings to ensure that your teams are compensated for their learning time.
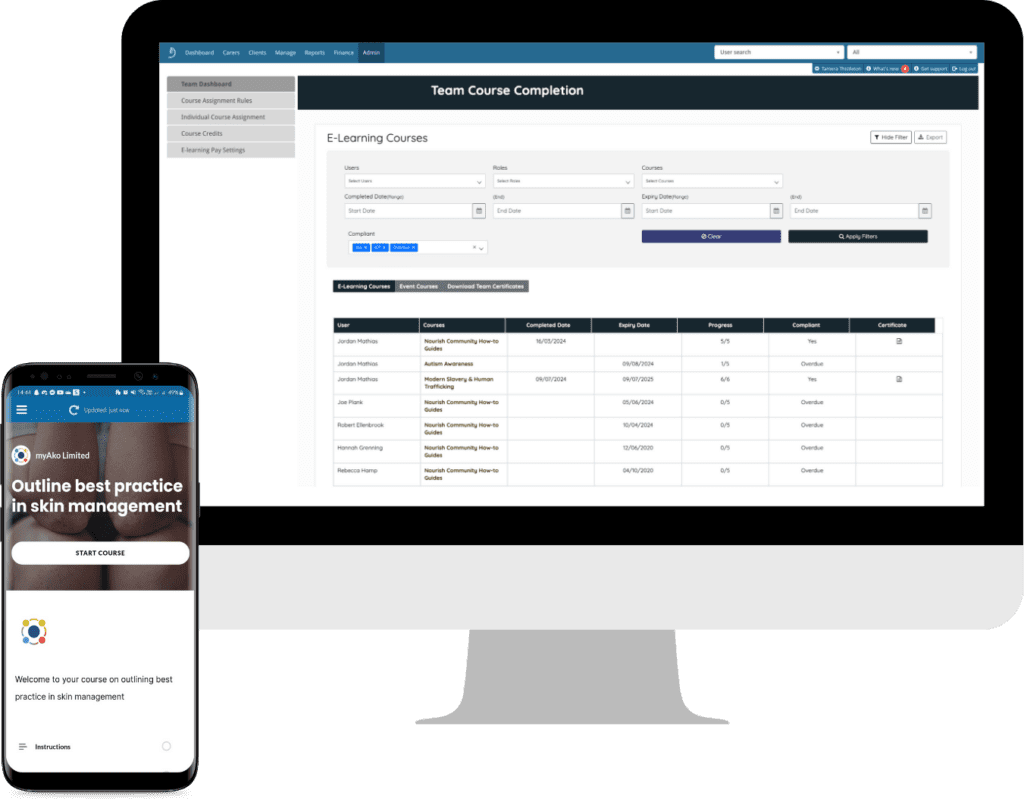
MyAko boasts a range of courses covering a variety of relevant topics for social care. Including professional skills, safeguarding and clinical best practise. With over 60 courses to choose from you can shape your training to the needs of your community. Here are some examples.
The Care Certificate is an agreed set of standards that define the knowledge, skills and behaviours expected of specific job roles in the health and social care sectors. Developed jointly by Skills for Care, Health Education England and Skills for Health because of the need for official certificates in our sector. The Care Certificate consists of the 15 minimum standards people considered ‘new to care’ need to cover which should form part of a robust induction programme. MyAko’s course covers the 15 standards within the Care Certificate and checks the knowledge of the learner through the end-of-module assessments.
MyAko offers courses that are directly tied to care skills, as well as ones that help develop other professional skills necessary to provide outstanding care. The appraisals course aims to provide the learner with general knowledge surrounding staff appraisal skills and the role it plays within the workplace. This course is a combination of both theoretical knowledge and interactive activities, designed to help the candidate learn, and practice. This develops crucial leadership and management skills for your staff and helps provide a pathway for further development.
Duty of Candour is a common expectation from all health and care providers. It requires care providers and managers to act in an open and transparent way with people receiving care or treatment from them. While this seems straightforward from the outside all carers can appreciate the delicate touch it requires. This course shows learners that promoting a culture of openness is a prerequisite to improving customer safety and the quality of our health and social care systems. Upon completion of the course, your team will be able to classify Duty of Candour and recognise best practice. Another key point is how you can distinguish between various levels of harm and associated actions and additionally which of these are notifiable safety incidents.
We recently released a new training matrix report. This report is available to all Nourish home care users, regardless of if you sign up for the new care eLearning courses. This exportable report provides an overview of your team’s training status, as a result making it easier to track who’s completed their training and who may need a refresher. For more information about your new report, log in to your Nourish Rostering system and check out the Training Matrix Report guide found in the Help Centre. With this new report we aim to make managing your team’s learning and development more efficient and straightforward.
Training is a crucial part of developing the future of care. It is vital we engage with professional development in social care to continue to take charge of our own sector. Empowered care teams deliver higher quality care with more job satisfaction. Investing in care eLearning can help with the recruitment and retention of your workforce as well. With Nourish and MyAko you can lay the foundations for your future success.
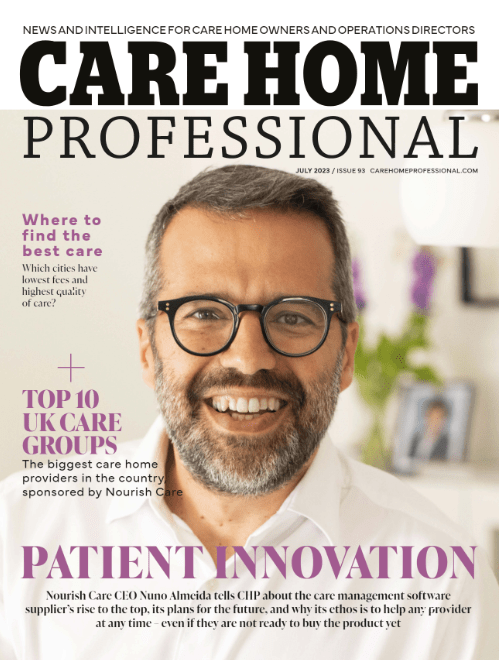
Our founder and CEO, Nuno Almeida, is featured on Care Home Professional’s cover for July 2023.
Nuno shares his thoughts on the social care sector, the growth and future of Nourish and how we align closely with the ambitions of our customers.
“We think we have the best product in the market. What makes the difference is our understanding of how a good digital product – with the right integrations, data science, sector knowledge, when all brought together – can translate into better outcomes for people needing care. We can do this from a single care home to hundreds of locations with a variety of types of care.”
Want to know more about how Nourish can work for you? Book a personalised demo with our team and see how Nourish can truly adapt to your care service.
We all understand the importance of valuing and respecting those we care for, when we speak about how you can truly deliver dignity in care, it might be hard to conjure up an exact idea of what that really means or looks like. Luckily Dignity in Care has come up with the 10 Dignity Do’s – an easy list that describes the values and actions of a high-quality care service that respects and upholds people’s dignity to the highest standard.
A Dignity Champion is a person who believes that being treated with dignity is a basic human right, not an optional extra. They believe that care provision must be: compassionate, person-centred, efficient and effective, and are willing to take action in order to achieve this.
“I have handed out Dignity in Care 10 Point ‘Dignity Do’s’ Cards to all staff in my care home – each time we have a team meeting we focus on one of the 10 Dignity Do’s and discuss what we can do to meet that challenge. Each meeting results in us making changes to the way we provide care.”
– A Dignity Care Champion
Dignity Champions are those in a care organisation that champion and uphold the 10 Dignity Do’s, as well as advocate and share the importance of dignity in any form of care. This includes:
You can find out more about becoming a dignity champion and the 10 Dignity Do’s by visiting Dignity in Care’s becoming a champion or register page. Another helpful resource is the Dignity Champion’s Toolkit for Action, which includes actionable insights, ideas and advice for people in a range of different care roles to help make a difference and bring dignity to care.
There are many ways that the Dignity Do’s can help care groups, teams and organisations improve their level of care and adapt to offer a continuously improving level of service. Championing the Dignity Do’s is only the start, we believe that in order to provide the highest quality care, moving to digital care planning enables you to create personalised care plans, record care accurately at the time of providing care and understand and act on trends about those you care for. By using digital, you can be much more efficient and spend more time providing person-centred, quality care.
To find out how care software and technology can be used to enhance your care service, or help you to better care for those you support, book a demo or get in touch with the team.
Thank you to Warrington Community Living for sharing the following article on their website. We love hearing how Nourish‘s digital platform is helping and improving care services across the country!