When Wes Streeting announced his three key shifts for the National Health Service (NHS) at the Labour Party Conference at the end of September social care’s ears were burning. A move from analogue to digital, hospital to community and sickness to prevention is a move towards care. Clearly social care has a big part to play in the future of the NHS. And technology plays a crucial role in the future of social care. When applied correctly digital solutions empower us to improve both efficiency and outcomes. Which offers care technology a central role in the government’s ongoing attempts to stage a digital revolution in health and care. We all know the why, given social care’s enduring challenges. It is uncovering the precise, who, what, when, and how of the matter that remains something of a mystery.
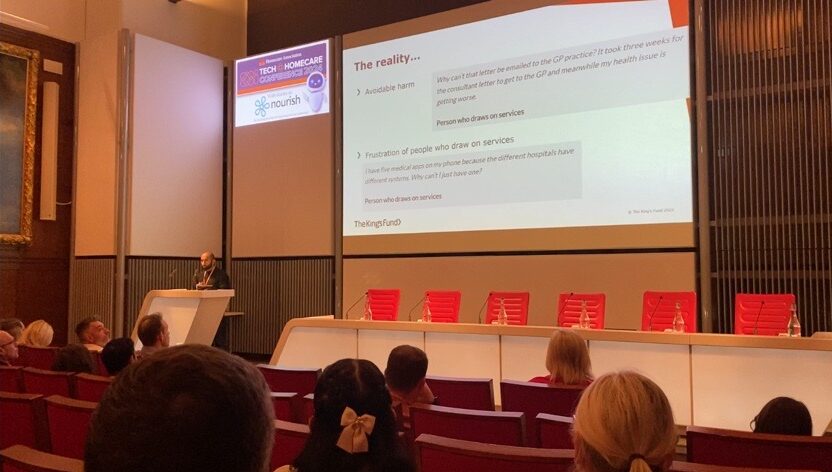
We recently headline sponsored the Home Care Association (HCA)’s Tech & Homecare conference. A day of insights, inquisition and understanding for leading home care providers and technology suppliers. On the day our CMO, Lee Gilbert, hosted a panel featuring a who’s who of digital rostering and AI suppliers discussing data, while The King’s Fund’s Pritesh Mistry joined HCA’s CEO Dr Jane Townson OBE to ask, ‘How can technology solutions help move care closer to home?’. The latter a conversation underpinned by the recently published, Nourish Care sponsored, study exploring ‘The reality of, and potential for, digitally enabled care in the community’. Reflecting the collaborative spirit of co-development that defines modern, outstanding care, these conversations detailed a variety of ongoing efforts to move social care from analogue to digital. Their success, their missteps, and the road still ahead.
Chair: Lee Gilbert, CMO, Nourish
Nuno Almeida, CEO, Nourish
Steve Sawyer, Managing Director, Access Group
Robin Batchelor, CEO, everyLife Technologies
Matthew Bond, CEO, Borderless
Abeed Mohammed, Co-founder, Birdie

There is already a wealth of positive examples of technology improving care quality. Providers applied digital solutions to a selection of the challenges they face. Both The King’s Fund research, and each of the panellists, presented their own positive instances. Pritesh detailed several different, key, areas that are already befitting from digital solutions, such as communication, care co-ordination and personalisation. Dr Townson added to this during their conversation, highlighting some Local Authority’s recent adoption of ‘magic notes’ as an example of technology changing people’s lives.
The panel built upon these cases with a specific focus on utilising existing data in systems. Matt Bond shared how Borderless share and aggregate data to pass benefits to individual people by finding the gaps in your existing service. The other four panellists all pointed to the efficiency their respective rostering platforms bring to care providers. When Robin Batchelor brought attention to the current inflection point in care technology it resonated around the room. Nuno Almeida agreed, “We’ve spent 14 years building the foundations. It’s not rocket science; the rocket science lies in your ability to react to needs.”
That is the crux of the matter, when we move from analogue to digital, we have to retain our focus on people’s needs. The ability to react to these needs is defined by our ability to engage with them. One of the biggest fears about moving from analogue to digital is based in the apprehension of losing the human touch that has always guided health and care in the UK. A fact reflected in two of the recommendations from the King’s Fund’s research. The need to ‘Shift culture to embrace the public’s digital capability’ and ‘Support staff to embed tech in their roles’. Neither of which are groundbreaking discoveries, but do require fresh ideas to address. Such as Scottish Care’s Care Technologist role. We know the potential of carers, their adaptability and commitment to any idea that can improve outcomes for their community.



What we need to do is make engaging with, and championing, care technology a simpler process. Which is not something that can be done overnight. “Asking people what is important to them is the biggest gap in our data,” admitted Nuno during the panel. “But this is also a big opportunity for us, asking, ‘What will really make a difference?’” The more we can involve people in the design process, the more ‘frontline’ feedback we can apply to our development. This co-production keeps people at the heart of care technology, which is crucial as we move to put technology at the heart of care.



Dr Townson concisely summarised this issue during her talk with Pritesh. ‘Technology for technology’s sake is not progress’. Innovation cannot be disruption in care, the standard approach for technology entering a new sector. The responsibilities are too great. We have to understand the barriers and develop enablers for adoption in the workforce and communities they support. Any one software solution aiming to promote wrap around care and support needs to ask itself a simple question. ‘How will the care providers work alongside our tech?’
Pritesh highlighted the need for this focus in his research with The King’s Fund. One of the recommendations from this research underlines the need to ‘develop strategies for co-developing digitally enabled services’. Specifically raising the point that developing a strategy for co-development and patient-led service design will help to direct digital service development and strategy. While this suggestion calls for action from ICSs, ICPs, the NHS and the Department of Health and Social Care (DHSC), it speaks to all digital suppliers and providers in social care. The move from analogue to digital in care must involve people at every step, or it is sure to get lost.
Nuno spoke about the need to ‘crawl, walk, then run, to get to data quality’. A process that rings true for all forms of digital technology. When The King’s Fund recommends ‘A national vision to guide local decisions’ it is not calling for a direct mandate. It is asking for a personalisable framework. ‘A guiding national vision, with local flexibility as to how it is achieved. One that will help to align the efforts of technology innovators, health and care providers, and leaders designing improved community-based services.’
The HCA’s conference was an example of just that endeavour. A selection of leaders, creators and providers sharing experiences and ambitions to help shape the future of care as we move from analogue to digital. One based in the commitment to collaboration that makes care the beating heart of our communities. After all, if you’re going to solve a mystery machine, it’s best to do it with a gang.
Technology in Social Care…
Since Kate Terroni became Chief Inspector this Summer, I have been reflecting on how a new person in that post would see their role in promoting innovation in the care sector. It was with childlike excitement that I read Kate’s latest blog post. In this, Kate describes how she has been shadowing some of her inspectors and her findings – and it was fantastic to get her initial thoughts on the use of technology by care teams.
“Speaking with carers I have found that this technology means they can spend more time with the people they support and less time doing paperwork — a welcome benefit of technology.”, Kate Terroni, Oct 2019
And what is the most refreshing is the clarity of thought on the difference between “using technology” and “innovation”, something that resonates immensely with how we see the world at Nourish.
We have long been believers that carefully designed technology, with the right associated services, can enable a whole range of cultural changes. Including how care teams perceive their own ability to drive innovation. It is important that care teams don’t develop a perception that innovation is something you buy. It is not.
Care teams showing CQC what good technology can achieve is a wonderful demonstration that technology makes a difference for them. It hasn’t always been this way.
Going forward it’s important to acknowledge that for a long time, many people misunderstood the potential for technology in Social Care. With a dozen challenges constantly putting pressure on care teams, the prospect of making a big change such as embracing digital tools for managing care has often filled people with dread – which is very understandable. And historically it wasn’t just for fear of change that care teams have put this off.
The maturity of the products available has come a long way in the last 5 years. Prior attempts to adopt technology by care teams invariably resulted in frustration – products that looked amazing in the eyes of a manager or the owner of a care home ended up requiring hours of training for care workers with clunky user experience, poor customer support, resulting in failed uptake, and a background feeling that “technology doesn’t work in social care”. Care workers were never heard in the process of choosing digital tools, and the introduction of technology was often done in the assumption that it would “help the numbers by making carers more efficient” – as if efficiency could be introduced by some sort of industrial process of optimisation. Thankfully, the sector and the technology that supports it have moved on.
Like any context that is as complex and nuanced as social care, the thought of designing technology at arm’s length resulted in oversimplified solutions often shaped within a software team which would then sell it as fast as possible – this was never going to work. So, what is it about social care that is so different from, say, healthcare? Why can’t we just use a personal health record and expand it?
Well, we can’t. We can’t because social care is not just about someone’s condition or frailty. Good social care services support the person as a whole. And people are extremely diverse – society as a whole is learning that there is no such thing as a template for an “older person” – as we have more people living longer our cultural stereotypes of what is an “older person” are crumbling – older people are “people” – we can’t stereotype them. And therefore, there is no universal template for an Older Person’s Care Plan. Good social care for a person living with frailty supports the person in a way that is aware of the whole person – not just of their frailty. And whereas a person has dozens of encounters with healthcare services in a year, the same person may have dozens of encounters with their care team in a single day.

Care Plans are as diverse as the people they are designed to support.
So, having spent 6 years continuously co-designing Nourish with hundreds of care providers, it’s no surprise care teams feel so different about us. We are not a “technology” company. We are a company that uses a software product and services to make care teams feel empowered to improve and innovate in the context of the care they provide. Carers don’t need to sit on training sessions for hours, it’s intuitive technology that allows them to understand the context of a person, know how to support and what’s important for the person, record naturally as part of providing support rather than “doing record keeping at the end of the shift”, and feel empowered. Empowered because they can spend more time with the people they support. And in addition, from knowing their residents better, they can continuously innovate, suggest adjustments to support plans, identify shifts in personal preferences or suggest new activities that are likely to improve the quality of life for each person.
Innovation happens when care providers design new and better ways to discharge people from hospital, or when they find different ways to enable people to go on a holiday, fulfil a last wish, increase their comfort, find or revive a sense of purpose, supporting every person, old and young, to be and feel the best they can feel.
Technology that enables care teams to do this, will be at the heart of all good care teams in the future. And we are delighted to see the Care Quality Commission so clearly sharing our vision on this.
Could technology help your care service?
Find out more about whether using an electronic care planning could help you and those you support here.
Moving away from what we know and stepping into the unknown can be a daunting experience. For both businesses and individuals, change isn’t easy and is often something we fear given it isn’t something that comes naturally; but should it be or should we actually fear just standing still? . In the words of Susan Jeffers sometimes we just need to ‘Feel the Fear and Do It Anyway’. This is particularly true when it comes to using digital in social care.
This notion of change and not being fearful of it is something that our founder and CEO, Nuno Almeida, touched upon at this year’s Care Show. Representing the ‘Care Software Providers Association’ (CASPA), Nuno addressed the issue of change in relation to the use of digital technology within the care sector.
Although more and more care services are adopting the use of digital technology, there is still an enigma that surrounds the evolution of it within the care sector. It’s hard to believe that in the UK, over 75% of care providers still use a pen and paper for planning and record keeping, rather than using electronic care planning systems. Whilst the care sector has evolved over the years, changes have been slow. There are still a lot of fears associated with digitalisation and its perceived risks. Key concerns revolve around:
All valid and understandable reasons as to why care providers are cautious of changing to a digital way of working. However, as Nuno raised the point, could paper present a bigger risk?
Records can be lost; information can be hard to find, and it can be hard to provide carers with context in terms of what is needed for those they are supporting. In the main paper records are seen more as a statutory obligation. A log of evidence to show standards of care to the likes of CQC and local authorities. The data isn’t being used in a way that can help us to improve and enhance care, something that digital technology can help overcome.
When records are input into a digital system, they become so much more than just evidence for inspection. They open up a whole new world of possibilities that simply wouldn’t be possible with stacks of paper. For example using an electronic care planning system to record digital records enables:
Clearly digital technology such as electronic care planning can provide care providers with a range of benefits, but how can the fear of change be overcome? Like with most things, when you are armed with the right information and the right guidance, change becomes less like something that should be feared and more like something that is manageable and exciting.
In Nuno’s words ‘with the right co-ordination, the right strategy and the right partners, we can get the right digital use in social care’ and this is one of the key aims of CASPA. To help promote and continue to grow the use of digital technologies in the social care sector to improve the quality of care delivered.
To ensure a smooth transition, there are a number of actions care providers can put into place to help when moving to electronic care planning. CASPA suggest the following guidance on how to source and implement digital transformation software.
So you’ve chosen the provider you want to use, but what next? Well you will need to consider how you will implement the new digital system. CASPA suggest following a three-step process for implementation:
Ensure you communicate with families and care teams in a way that is reassuring and clear about the reasons for adopting digital. Try to build excitement and show that this change is positive and something that they don’t need to be nervous about.
Agree whether your chosen supplier will train all your staff or just your internal training team who will then deliver the training to the remaining members of your staff. Once this has been agreed deliver your training accordingly. Give your team reassurance that they can tackle and deal with the change and help them to feel in control by showing them that there are clear plans in place for training and roll-out.
Agree how devices are prepared and deployed. Tell staff where they need to be and when. Ensure you know how user accounts are created and how records are created for the people you support.
Good providers will be able to provide you with all the information you and your team need to ensure you are comfortable and ready for the transition to digital. From giving you clear guidance about GDPR responsibilities to how to manage devices and lock them down should they go missing. When looking for a provider CASPA recommends asking the following questions to help you find out whether they would be a good fit for you:
About the Care Software Providers Association (CASPA)…
CASPA has been established in the UK as an independent, not for profit, member-driven association. The association is currently led by a volunteer group of founding board members, each of whom manages a well-established software company that provides solutions for social care providers
CASPA Mission…
Find out more about whether using an electronic care planning could help you and those you support here.
The retired and ageing hold two invaluable commodities time and knowledge. With employment, affordable housing and free university education, the older generation accumulated a large amount of social capital, in the form of knowledge and connections. By recycling this social capital attained by the ageing generation we could facilitate significant benefits for society.
There is a common characterisation that the ageing population is further increasing pressures on our healthcare services and could even lead to a financial burden at the individual level. This idea is heavily enforced by our media, that has continually prompted us into this way of thinking. The Guardian, for instance, suggests that 2.8 million people over the age of 65 will need nursing and social care by 2025.
There seems to be an over-reporting of potential financial costs, setting the trap for a simplistic argument. This focus on portraying a whole generation in terms of ‘financial costs’ only leads other generations to be concerned with the future ‘financial burden’ they may find themselves facing.
Instead, we should be capitalising on the wealth of knowledge and experience that this older generation has to offer society. We should be focused on sharing knowledge across generations, looking to our elders to offer their expertise built over a lifetime of experience.
By adopting this mindset and starting to ask different questions we, as a society, could start to nurture significant rewards.
How often do we complain that there is not enough ‘real -life experience’ taught in schools?
We can create schemes where those who have this experience partner and interact with those who are learning and starting their way in the world. Both parties can learn from each other, helping foster understanding and mutual respect by altering perceptions between the generations.
Charities too are always in need of people from all different experiences and backgrounds. Widening the experience pool in the third sector can only help the interaction across sectors and better aid the end users of the charities focus.
—
Entering the world of work can be extremely challenging. Young professionals often have no experience – whilst the retired have experience, knowledge and more often than not, time. This social capital needs to be passed on.
Mentoring is an amazing and currently undervalued way of passing on knowledge and advice. These sorts of programs would be incredibly rewarding as they could positively impact people’s futures. Imagine the innovation and growth we would see by leveraging the experience of those that have gone before us.
—
Parents and grandparents have what is often an underappreciated role in society for providing parental and pastoral support. Helping to take care of others and nurture their growth is a highly rewarding pastime and has many social and psychological benefits.
It also would help to ease the ‘workload’ on an increasing number of families and single parents who are trying to balance the pressures between work and family. This would allow younger generations to have careers and further their professional lives; working to increase household incomes and further boost the economy.
AgeUK has illustrated the importance of staying active, both physically and mentally, and how being ‘switched on’ can be led to a healthy, longer life. What better way to remain active and social than by utilising all of the experience you have pulled together in your life and sharing that with others.
Mentoring, for example, is both highly rewarding and requires ongoing cognitive function to stimulate the mind. What a brilliant way to foster cross-generation dialogue and start to break down our inter-generational prejudice.
It’s also well known that as we age, we lose many social connections. This can lead to feelings of isolation and loneliness. Bringing generations together, we can build new relationships and networks and help to ensure everyone has that all-important social structure.
The retired and ageing hold two of the most valuable resources in life, experience and knowledge. They also often have the time to invest in sharing that with others. As a society we could be tapping into this resource, sharing the social capital this group has attained with the younger generations. Over time, imagine the positive outcomes we would see.
—–*—–
You may also be interested in reading:
Drop us a message to find out more about our electronic care planning and recording of daily notes.